https://www.malone.news/p/declassified-documents-link-us-bioweapons
Declassified Documents Link U.S. Bioweapons Program to Lyme Disease Outbreak
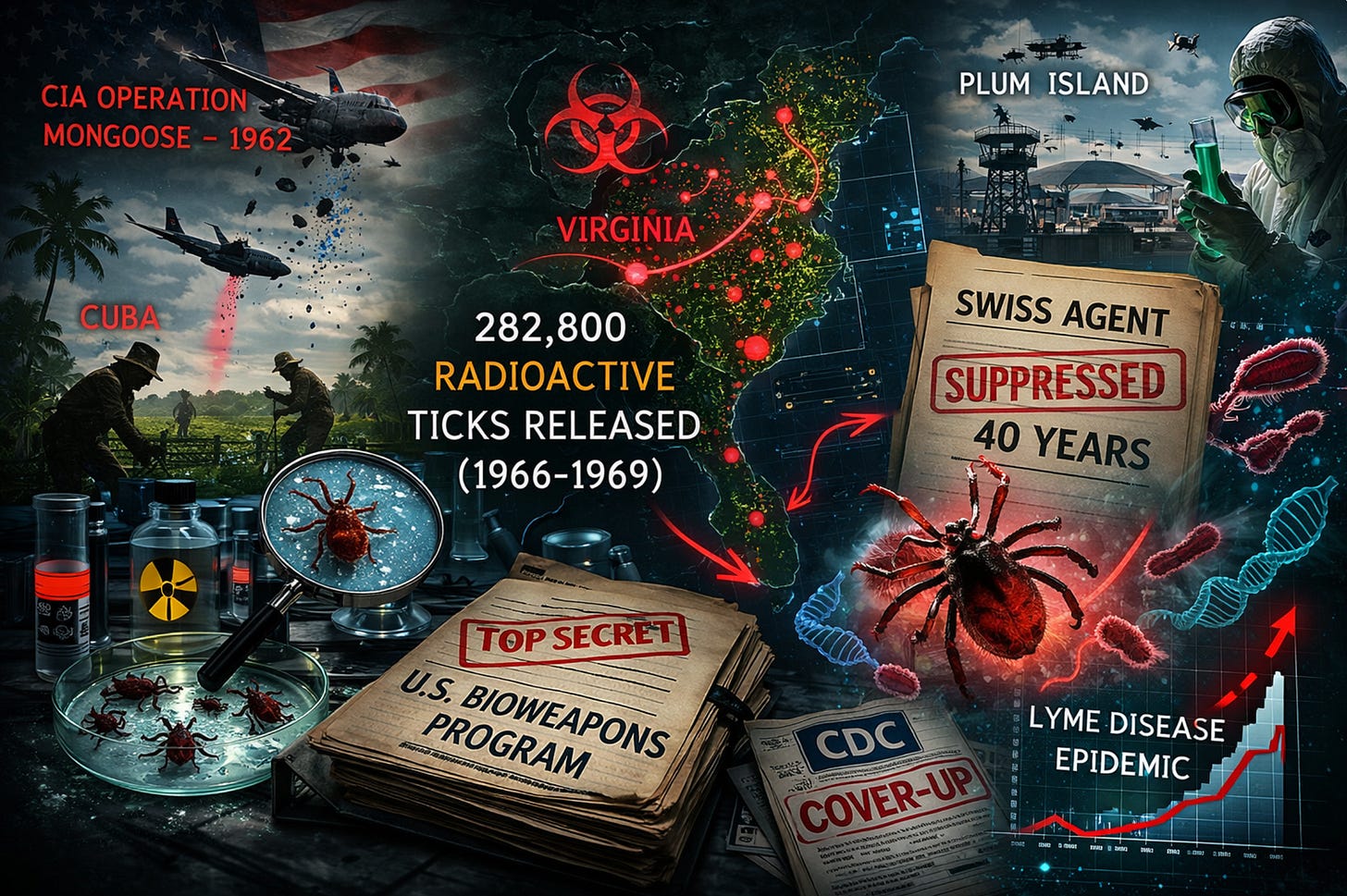
Exclusive: Military released 282,800 radioactive ticks, suppressed co-infection research for 40 years
An extensive investigation based on declassified government documents and previously suppressed scientific research has uncovered compelling evidence that U.S. biological weapons programs contributed to the emergence of Lyme disease, which now affects hundreds of thousands of Americans annually.
The investigation reveals a pattern of concealment spanning six decades, including the systematic suppression of critical medical research and the release of nearly 300,000 radioactive ticks across Virginia to study how the disease-carrying insects would spread.
CIA Deployed Infected Ticks Against Cuba
Declassified documents and testimony from a CIA operative describe the 1962 deployment of infected ticks against Cuban sugarcane workers as part of Operation Mongoose, the Kennedy administration’s effort to destabilize Fidel Castro’s regime.
The operative, now in his seventies, told researchers that the “strangest thing he ever did was drop infected ticks on Cuban sugarcane workers” using C-123 transport aircraft flying nighttime missions “almost skimming the surface of the Caribbean to avoid Cuban radar.”
After returning from Cuba, the operative’s four-month-old son developed life-threatening fever requiring emergency surgery. His CIA commander advised him to “burn all the clothes you took to Cuba. Burn everything,” indicating contamination concerns.
The deployment was canceled when “Cuba’s shifting winds made accurate payload delivery difficult,” according to the operative’s account.
Massive Domestic Tick Experiments
Between 1966 and 1969, the U.S. military released 282,800 lone star ticks made radioactive with Carbon-14 across Virginia sites along bird migration routes. The radioactive marking allowed researchers to track the ticks’ spread using Geiger counters over several years.
Before these experiments, lone star ticks were not found above the Mason-Dixon Line. Within years of the Virginia releases, they had established populations on Long Island for the first time. Two tick experts consulted about these releases said they “were aghast” and “you’d never be able to do that now.”
The Swiss Agent Cover-Up
In 2014, researchers discovered extensive unpublished materials in the garage of deceased scientist Willy Burgdorfer, who identified the bacterium that causes Lyme disease. The materials revealed that Burgdorfer had found a second pathogen called “Swiss Agent” in Lyme patient blood samples from Connecticut and Long Island in the late 1970s.
Blood from Lyme patients showed “very strong reactions” to Swiss Agent testing, but this finding was completely omitted from Burgdorfer’s landmark 1982 study that identified the Lyme disease bacterium. The suppression of this research for over 40 years may have contributed to treatment failures in chronic Lyme patients.
Dr. Jorge Benach and Dr. Allen Steere, co-authors of the 1982 study, now acknowledge that Swiss Agent research “should be done” because “public health concerns warrant a closer look.”
Project 112: The Hidden Bioweapons Expansion
Defense Secretary Robert McNamara authorized Project 112 in 1962, creating what researchers describe as a bioweapons program “almost as large and secretive as the Manhattan Project.” The program involved 134 scheduled tests from 1962-1974 with production facilities capable of breeding 100 million infected mosquitoes monthly and 50 million fleas weekly.
The program’s existence was “categorically denied by the military” until 2000, when a CBS News investigation forced acknowledgment. Documents show the program involved “every branch of the U.S. armed services and intelligence agencies” with testing sites spanning multiple countries.
Operation Big Itch in 1954 successfully deployed 670,000 fleas from cluster bombs, proving arthropods could survive aerial deployment and “soon attached themselves to hosts.” The test validated bioweapons capable of covering “a battalion-sized target area and disrupt operations for up to one day.”
The Plum Island Connection
Plum Island Animal Disease Center sits just 13 miles from Lyme, Connecticut, where the disease was first identified. From 1952-1969, the facility was managed by the Army Chemical Corps for biological warfare research before transfer to the Department of Agriculture.
The facility “frequently conducted its experiments out of doors” with acknowledged containment failures where “test animals mingled with wild deer, test birds with wild birds.” Richard Endris maintained “over 200,000 soft and hard ticks of varying species in tick nurseries on Plum Island, personally collected from locations as far away as Cameroon, Africa.”
Wildlife regularly moved between Plum Island and the mainland. “Deer from Lyme regularly swam to Plum Island, and local birds flew there to feed on insects,” creating direct pathways for laboratory pathogens to reach wild populations.
Disease Emergence Timeline
The Long Island Sound region experienced an unprecedented outbreak of tick-borne diseases beginning in 1968:
- 1968: First Eastern U.S. human babesiosis cases appear on Nantucket
- 1968: Rocky Mountain spotted fever appears in Cape Cod region
- 1970: Hundreds of Rocky Mountain spotted fever cases documented on Long Island
- 1972: First 51 documented Lyme arthritis cases in Old Lyme, Connecticut
“By the 1990s, the eastern end of Long Island had by far the greatest concentration of Lyme disease,” according to one analysis. “If you drew a circle around the area of the world heavily impacted by Lyme disease, the center of that circle was Plum Island.”
Burgdorfer’s Cryptic Admissions
Willy Burgdorfer, who discovered the Lyme disease bacterium in 1982, spent most of his career developing tick-borne biological weapons before transitioning to civilian research. In 2013 video testimony, he confirmed participation in bioweapons research and “insinuated there had been an accidental release of some sort.”
After cameras stopped rolling, “Willy told us with a smile, ‘I didn’t tell you everything.’ But try as we might, we couldn’t get him to say more.” Before his death in 2014, he left a note stating “I wondered why somebody didn’t do something.”
In 2007, when documentary filmmakers attempted to interview Burgdorfer, a government scientist “pounded on the door” demanding to “sit in on this interview,” indicating ongoing official concern about his potential disclosures.
Pattern of Institutional Concealment
The investigation identified systematic concealment behaviors spanning multiple decades:
- Project 112 denied for 50 years despite extensive documentation
- Swiss Agent research suppressed despite public health relevance
- Relevant documents kept classified long after security justifications expired
- Congressional investigation requirements resisted
- Laboratory origin questions characterized as “conspiracy theories”
(See link for article & comprehensive integrated multi-layered analysis of the issue)
_____________
**Comment**
An AI-enhanced retrospective analysis found:
- phylogenetic gaps between ancient strains and the strains that emerged in the 60’s & 70’s (in other words, what we are infected with isn’t found in nature – it’s been tweaked in a lab)
- co-infection clustering of three distinct diseases in the same geographical area and timeframe (but are never even considered, discussed or treated)
- GMO signatures
- distribution anomalies inconsistent with natural tick migration patterns (And it ain’t from climate change! It’s from man-made tick redistribution out of airplanes & migrating birds & animals)
- suppression of the Swiss Agent indicating systematic research concealment
In short, it’s wide-spread systemic fraud perpetrated upon an unsuspecting public, yet the answer always presented is to have the very agencies behind this fraud do an investigation on themselves! It will never happen. ‘Dog and pony show’ comes to mind.
We’re on our own and the quicker we embrace this salient fact, the quicker we will get better.
For more:
- https://madisonarealymesupportgroup.com/2020/09/25/why-should-we-care-about-lyme-disease-a-colorful-tale-of-government-conflicts-of-interest-probable-bioweaponization-and-pathogen-complexity/
- https://madisonarealymesupportgroup.com/2019/02/22/why-mainstream-lyme-msids-research-remains-in-the-dark-ages/
- https://madisonarealymesupportgroup.com/2024/03/11/lyme-another-perfect-bioweapon/
- https://madisonarealymesupportgroup.com/2024/05/31/history-of-bioweapons-lyme-disease-and-the-question-of-virology-dr-lee-merritt-adam-finnegan/
- https://madisonarealymesupportgroup.com/2024/05/14/uncensored-was-lyme-disease-created-as-a-bioweapon/
- https://madisonarealymesupportgroup.com/2026/01/23/how-ticks-became-bioweapons/
- https://madisonarealymesupportgroup.com/2018/12/19/its-1984/
- https://madisonarealymesupportgroup.com/2023/05/25/lyme-disease-mycoplasma-and-bioweapons-development-timeline/
- https://madisonarealymesupportgroup.com/2024/02/13/the-sleeper-agent-the-rise-of-lyme-disease-chronic-illness-and-the-great-imitator-antigens-of-biological-warfare/
- https://madisonarealymesupportgroup.com/2019/07/19/biological-warfare-experiment-on-american-citizens-results-in-spreading-pandemic/