By Lindsay Christensen, MS, CNS, LDN, CKNS
Your immune system, brain, and gastrointestinal system, not to mention the rest of your body, require optimal nutrition to function properly.
Improving nutrition can help your body fight Lyme disease, allow your immune system to work optimally and reduce the adverse effects of Lyme disease (and Lyme treatments) on the gut, brain, musculoskeletal system, and hormones.
Unfortunately, nutrition is often placed on the back burner and sometimes wholly overlooked in Lyme disease treatment protocols
Why does nutrition matter for Lyme disease recovery?
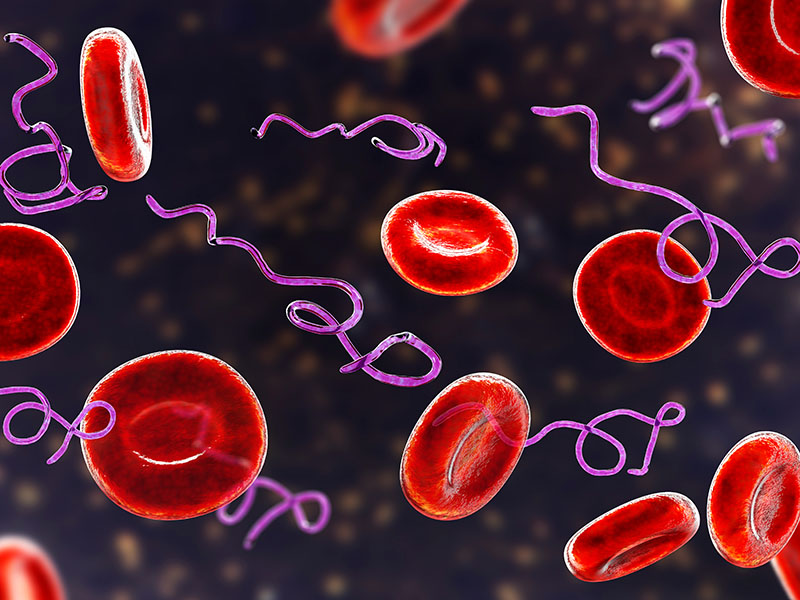
Lyme disease, contracted from the bite of an infected tick, is one of the fastest-growing infectious diseases in the United States. At least 476,000 people are diagnosed with and treated for Lyme disease annually in the nation. Up to 1.5 million people in the U.S. may suffer from persistent symptoms of the illness.
I count myself among those 1.5 million people with chronic Lyme disease. After an arduous four-year battle with a mysterious chronic illness, I was diagnosed with Lyme in my early twenties.
However, my journey wasn’t over once I received my Lyme diagnosis. Instead, this was just the beginning of a multi-year trek through countless Lyme disease treatments. While I saw some improvements, it wasn’t until I took my nutrition seriously that I saw significant, sustainable progress in my health.
 This led me to pursue my Master of Nutrition in Human Nutrition, become a clinical nutritionist, and ultimately specialize in working with clients who have Lyme disease. I have also written a book called The Lyme Disease 30-Day Meal Plan: Healthy Recipes and Lifestyle Tips to Ease Symptoms.
This led me to pursue my Master of Nutrition in Human Nutrition, become a clinical nutritionist, and ultimately specialize in working with clients who have Lyme disease. I have also written a book called The Lyme Disease 30-Day Meal Plan: Healthy Recipes and Lifestyle Tips to Ease Symptoms.
While nutrition alone cannot cure Lyme disease, it can significantly ease your symptoms, accelerate your healing process, and create a stronger, more resilient body capable of healing from Lyme. In addition, nutritional treatment is a powerful complement to both antibiotic and herbal protocols for Lyme disease.
For the Lyme patient struggling with treatment decisions, chronic fatigue, pain, and brain fog, sorting through nutrition information to figure out what to eat can feel daunting. Let’s discuss five steps you can take starting today to maximize your nutrition and support Lyme disease recovery.
Step 1: Remove inflammatory foods
Infection with Borrelia and co-infections induces a profound inflammatory response in the body. This can affect the gut, joints, brain, cardiovascular system, eyes, and skin.
When working with clients who have Lyme disease, I begin by having them remove the most common dietary inflammatory triggers, including:
- Processed foods
- Refined carbohydrates and sugar
- Industrial seed oils, such as canola, corn, cottonseed, soybean, and safflower oils.
Refined carbohydrates and added sugars, such as cane sugar and high-fructose corn syrup, also promote the growth of inflammatory gut bacteria.
Between 70 and 80 percent of your immune system resides in your gut, so when your gut microbiota is unhealthy, your immune function and thus your ability to combat Lyme disease will suffer. Removing refined carbohydrates and added sugars is essential for reducing inflammation and regulating the immune system in Lyme.
I also find that many of my clients do best avoiding gluten and conventional dairy products from grain-fed, industrially-raised animals, since both of these foods are potent inflammatory triggers.
Step 2: Eat anti-inflammatory foods
In addition to removing inflammatory foods from our diets, we also need to incorporate foods that actively reduce inflammation. Work on including the following anti-inflammatory foods into your diet:
IL-17 is a pro-inflammatory cytokine (an immune signaling molecule) made by the immune system during Lyme infection. However, chronic IL-17 production can promote rampant inflammation and even autoimmunity. Metabolites of omega-3 fatty acids called “specialized pro-resolving mediators” or SPMs, blunt the production of IL-17 and can thus help calm the inflammatory response.
Try to eat several servings of fatty cold-water fish per week to bolster your omega-3 intake. Choose from the “SMASH” seafood, which are low in mercury and high in omega-3’s. SMASH stands for “salmon, mackerel, anchovies, sardines, and herring.”
Cruciferous vegetables, such as broccoli and cauliflower, contain compounds called glucosinolates that increase the body’s glutathione production.
Glutathione, an antioxidant and immune-signaling molecule, plays a crucial role in the immune response to Borrelia.
Borrelia spirochetes stimulate macrophages, including glial cells in the brain, to release the inflammatory cytokines IL-6 and TNF-α. Excessive production of these molecules has neurotoxic effects on the brain.
In animal studies, blueberries have been found to reduce IL-6 and TNF-α production and may thus help protect the brain and dampen overall inflammation.
Oleuropein, a major component of extra virgin olive oil, also reduces the production of the inflammatory cytokines IL-6 and TNF-α involved in the Lyme-induced inflammatory response. Be sure to choose organic olive oil to avoid consuming pesticide or herbicide residues, which have immune system-disrupting effects.
Step 3: Support your immune system
Your immune system requires an array of nutrients to function at its best. Furthermore, infection and stress deplete the body of critical micronutrients. Let’s take a look at several of the micronutrients needed for a well-functioning immune system:
Vitamin D is frequently low in patients with persistent Lyme disease On top of that, Borrelia burgdorferi directly reduces vitamin D receptor expression in immune cells, increasing the need for vitamin D.
Vitamin D is critical for Lyme disease recovery. Daily sun exposure and the consumption of vitamin D-rich foods, including fatty cold-water fish and pastured egg yolks, support a healthy vitamin D status. However, supplementation is often necessary, especially during the fall and winter months.
Vitamin A is a fat-soluble vitamin (a vitamin that dissolves in fats and oils) that regulates both the innate and adaptive branches of the immune system. The innate immune system is our set of frontline immune defenses, whereas the adaptive immune system is composed of specialized cells that target specific pathogens.
We need both branches of the immune system to battle Lyme, and vitamin A can help. Interestingly, vitamin A deficiency worsens Lyme arthritis in mice, whereas vitamin A replenishment reduces the harmful inflammatory response.
Retinol, the form of vitamin A the immune system requires, is found only in certain animal foods, such as egg yolks and liver. In addition, your body can create retinol from carotenoids, vitamin A precursors in yellow and orange plant foods, such as winter squash and carrots. However, this conversion process is not efficient in many people, necessitating vitamin A intake through animal foods.
Zinc is the second most abundant micronutrient in our bodies after iron. It plays several roles in the immune system, including supporting the intestinal barrier, the layer of cells that lines the gut and maintains the intestinal immune system.
Zinc also inhibits complement activity. Complement is a part of the immune system that is excessively activated by Lyme infection and contributes to inflammation.
The World Health Organization reports that one-third of the world’s population is at risk for zinc deficiency. Vegans, vegetarians, the elderly, and those with gastrointestinal issues that compromise nutrient absorption are particularly at risk for deficiency. To support your immune system, emphasize foods rich in zinc, including oysters, red meat, organ meats, and poultry.
Step 4: Support your gut health
Many individuals with Lyme disease have gone through multiple rounds of antibiotics. While antibiotics can offer significant benefits to many Lyme sufferers, they also reduce levels of beneficial microorganisms in the GI tract. This allows less desirable opportunistic and pathogenic organisms, including various yeasts and bacteria, to proliferate.
The resulting imbalance in the gut microbiota can compromise immune function, digestion, and nutrient absorption. Furthermore, preliminary research suggests that Borrelia may directly infect the gastrointestinal tract. It is thus crucial to support the health of your gut if you have Lyme disease.
A growing body of research indicates that diet profoundly impacts gut health. There are certain foods you should prioritize to support your gut health, including:
- Fiber: Dietary fiber found in vegetables, fruits, nuts, seeds, and legumes supports the growth of beneficial gut bacteria, which positively impact our immune function and digestion.
- Fermented foods: Fermented foods, such as sauerkraut, kimchi, beet kvass, and yogurt (for those who tolerate dairy products), provide probiotics that support gut health and immune function. Try to consume a serving of fermented foods daily. Remember to rotate fermented foods since each food offers unique probiotic microorganisms and health benefits.
- Bone broth: Bone broth is a slow-cooked broth made from boiling animal bones and connective tissues in water. It is gelatinous and rich in glycine and proline, amino acids that help create a healthy gut. I encourage my clients with Lyme disease to consume bone broth regularly to support intestinal health.
Step 5: Support your joints and brain
Borrelia can cause extensive damage to collagenous tissues in the body, such as skin, tendons, and ligaments. Vitamin C is a cofactor for enzymes involved in collagen synthesis. Optimize your vitamin C intake by consuming foods such as bell peppers, citrus fruits, berries, and broccoli.
The brain is severely affected in many cases of chronic Lyme disease, referred to as “neuroborreliosis.” Lyme infection promotes brain inflammation and impairs energy production in neurons, making it difficult to think clearly and maintain a balanced mood.
Vitamin B12 and DHA are two nutrients necessary for healthy brain function. B12 is supplied through meat, poultry, fish, and eggs, while DHA is an omega-3 fatty acid that we can consume through seafood, such as wild salmon and sardines.
There are many other nutritional factors that can support healthy brain function in Lyme disease, but vitamin B12 and DHA intakes are two of the most important.
Try a recipe from my book
Sesame Chicken Salad
This refreshing salad manages to be both sweet and savory, with a lovely crunch thanks to the addition of slivered almonds. It requires very little prep time, especially if you make the shredded chicken ahead of time in a slow cooker.
The short amount of prep time required is perfect it you’re short on time or energy for cooking. This salad contains several functional food ingredients beneficial for those with Lyme disease, including vitamin C-rich oranges and lime juice, folate-rich leafy greens, and anti-inflammatory extra-virgin olive oil.
Prep Time: 10 minutes
Dairy-Free, Gluten-Free
Ingredients:
FOR THE SALAD:
- 3 cups mixed greens
- 4 ounces cooked chicken breast
- 2 tablespoons slivered almonds
- ½ cup sliced cucumber
- 1 cup fresh orange segments
- 2 scallions, chopped
FOR THE DRESSING
- 1 tablespoon toasted sesame seeds
- 1 teaspoon peeled and grated fresh ginger root
- 2 tablespoons tamari sauce (be sure to select gluten-free tamari sauce)
- 2 tablespoons rice vinegar
- 1 tablespoon honey
- 1 scallion, finely chopped
- Juice of ½ lime
- 1/3 cup extra-virgin olive oil
- ¼ cup freshly squeezed orange juice
- 2 teaspoons toasted sesame oil
- In a large mixing bowl, combine the greens, chicken, almonds, cucumber, orange, and scallions.
- In a glass jar or other lidded container, combine the sesame seeds, ginger, tamari sauce, rice vinegar, honey, scallions, lime juice, olive oil, orange juice, and sesame oil. Cover and shake well.
- Add the dressing to the salad and gently toss to coat.
- Serve immediately or refrigerate the salad and dressing in separate airtight containers for up to 2 days.
Lindsay Christensen has a Master of Science in Human Nutrition and is a Certified Nutrition Specialist and Licensed Dietitian Nutritionist. In her private clinical nutrition practice, Ascent to Health, she specializes in nutrition care for individuals with Lyme disease and other environmental illnesses.