How Long Does It Take For Herbal Supplements to Work?
https://vitalplan.com/blog/how-long-does-it-take-for-herbal-supplements-to-work?

Reviewed by Bill Rawls, MD
Medical Director of Vital Plan
Questions Answered
- How Long Does It Take for Herbal Supplements to Work?
- Can I Take Herbal Supplements With Prescription Drugs?
- Which Is Better: Whole Herbs or Extracts?
- Can Herbs Cure My Illness?
- Since Herbs Are Natural, Does That Mean Herbal Supplements Are Safe?
- Is It Possible To Take Too Many Herbs?
- Are Herbal Supplements Regulated by the FDA?
- How Can I Tell if a Supplement Is Good Quality?
- Does Insurance Cover Alternative Medicine?
Herbs have been used for thousands of years all over the world to address every imaginable health concern, and the amount of research supporting their powers grows every day. And yet their role in modern medicine is still minimized: Herbal therapy isn’t part of the curriculum in traditional medical school, and so most doctors don’t have the training to answer even the most common questions about herbs.
And if you’re new to herbs, or even if you’ve been taking them for a while but have a new health concern or circumstance like a new drug prescription, questions are bound to come up. “Hardly a day goes by that someone doesn’t ask me how long it takes to get results from a certain herb, or if they need to worry about taking a too-high dose,” says Dr. Bill Rawls, medical director of Vital Plan.
So, we’ve asked Dr. Rawls to tackle these and other top herbal questions here to get you the intel you need to put herbs to work for you.
How Long Does It Take for Herbal Supplements to Work?

Herbs have some amazing capabilities — but they aren’t magic pills. “The amount of time it takes to see results is somewhat variable, but typically it’s much slower than a pharmaceutical,” says Dr. Rawls.
That’s because pharmaceutical drugs are generally designed to activate or block a dysfunctional process in the body that is triggering symptoms or illness, whereas herbal supplements work to resolve the dysfunctional problem itself. For instance, heartburn medications work by blocking the natural process of producing the stomach acids that are making you uncomfortable — they’re a stopgap, but not a true solution.
By comparison, herbs like slippery elm bark, berberine, and dandelion extract help stop the underlying causes of reflux by nourishing the lining of the GI tract, balancing the gut microbiome, and restoring normal communications between gastrointestinal cells. “With herbs, there’s more of a process of healing involved, and that takes time,” Dr. Rawls explains.
That said, some herbs — called effectors — have a specific targeted action, and alleviate symptoms within an hour or so, says Dr. Rawls. One example is lily of the valley; it’s often used for cardiovascular problems like heart failure or irregular heartbeat. (Note that lily of the valley should only be used under physician supervision to avoid toxic doses.)
Still, for the most part, herbs are restorative, which means patience and persistence is key to seeing significant and lasting results. “Restorative herbs may have a small immediate effect, but can take weeks or months to build up in your system enough for you to really notice that long-term healing process and longer-lasting benefits,” says Dr. Rawls.
Can I Take Herbal Supplements With Prescription Drugs?

The short answer: Probably — with the caveat that you should always consult with your healthcare practitioner before taking any new herb or treatment. “But the potential for a bad interaction is pretty small,” says Dr. Rawls. That’s because most herbs and drugs function very differently and affect different parts of the body, so they’re not typically interacting at all.
On the contrary, herbs can sometimes be an effective complement to medications. Consider berberine, andrographis, garlic, and reishi mushroom, for example: They all help promote a balanced gut microbiome, making them a nice complement to antibiotics, which can throw the gut microbiome out of whack.
But as always, there are exceptions to the rule, and taking certain herbal supplements with prescription drugs can have some dangerous side effects, as well as impact the efficacy of the drugs, according to a small study in the British Journal of Clinical Pharmacology. “The biggest concern is if you’re on blood thinners, because most herbs are blood thinners as well,” says Dr. Rawls.
Other medications that might interact with herbs include SSRI antidepressants, prescription sedatives, sleep aids, anti-anxiety medicines, thyroid hormones, and diabetes medications. If you’re taking one of these — or any prescription drug — do your research carefully and consult with your doc before adding herbs to your regimen.
Which Is Better: Whole Herbs or Extracts?

There’s nothing wrong with whole herbs, but you’re going to get more bang for your buck with herbal extracts.
“What we’re interested in with herbs is their phytochemistry, the natural chemical substances called phytochemicals that have antimicrobial, anti-inflammatory, and antioxidant powers, among others,” says Dr. Rawls. “We’re less interested in the stems, roots, and leaves. When they’re dried out and ground up into a fine whole-herb powder, a high percentage of what you’re getting is fiber, not phytochemicals.” That makes whole herbs less expensive, but also less potent.
With extracts, you’re removing the phytochemicals from the plant and leaving behind what’s unnecessary, says Dr. Rawls. Liquid extracts (aka tinctures) are made by soaking the whole herb in a solution of water and alcohol or another liquid like vegetable glycerine or apple cider vinegar; they’re taken orally and absorbed in the intestines. Powdered extracts are the most potent: They’re made by soaking the herb in a solvent that’s later evaporated and then packed into a super-concentrated capsule or tablet.
Can Herbs Cure My Illness?

Federal regulations do not allow herbal supplement companies to make any medical claims. As such, herbs can’t be marketed as a treatment, cure, or any other kind of disease prevention.
But herbs’ actions can promote homeostasis, a healthy, stable internal environment within the body that allows for proper functioning, which may help an illness to be resolved, says Dr. Rawls. He explains that herbs do three big things that contribute to wellness:
- Suppress microbes like bacteria, fungi, and viruses that are present in our tissues and compete with our cells for vital resources
- Protect cells from damaging and inflammation-causing free radicals
- Promote communication between our cells
“All three actions boost cellular function, and when your cells are functioning optimally, you’re more likely to avoid things like inflammation and bacterial overgrowth that contribute to a number of illnesses and diseases,” says Dr. Rawls.
Since Herbs Are Natural, Does That Mean Herbal Supplements Are Safe?

Yes, herbs are natural, and because they’re more like food, their potential for toxicity is extraordinarily low. That’s especially true when compared to synthetic pharmaceutical drugs, which have a higher potential for toxicity and side effects. (Note that plant-based supplements are very different from sports or performance-enhancing supplements, some of which have been found to contain banned or harmful substances.)
Even so, there are a few exceptions to be aware of. Effector herbs like kava kava and cannabis in the form of marijuana have more drug-like qualities, and so they can become toxic with chronic and heavy use.
Remember, too, that some herbs do interact with medications and cause unwanted side effects. St. Johns’ wort, for instance, which has been shown to be effective for easing mild to moderate depression and menopausal symptoms, can also reduce the effects of antidepressant and anti-anxiety medications.
And some herbal supplement labels worn against taking the contents if you’re pregnant or nursing. That’s not because herbs are unsafe, but there are a few that should be avoided by certain populations because of the way they are processed by the body..
Ultimately, according to federal regulations, supplement companies are responsible for providing evidence that their dietary supplements are safe and for ensuring that product labels are not misleading. So do your research to find a company you trust, read the label so you know what’s inside the bottle, and ask your healthcare provider how it may react with any other supplements and medications you take.
Is It Possible To Take Too Many Herbs?

Not usually. Even in large doses, few herbal substances can actually kill you. “Plants produce phytochemicals to protect their own cells, and the phytochemicals in herbs mesh particularly well with our own biochemistry,” says Dr. Rawls. “When we consume the herbal phytochemicals, our cells benefit from those protective mechanisms.”
The toxic dose for most herbs is very high, says Dr. Rawls — especially compared to pharmaceuticals, which can be lethal even in small amounts. However, you do want to be careful with certain effector herbs like St. John’s wort, which has more potential to cause issues such as agitation, anxiety, and insomnia in high doses.
If you do take too much of a restorative herb, though, you’re likely to get a stomach ache or feel a little nauseous, but it won’t otherwise hurt you, Dr. Rawls adds.
Are Herbal Supplements Regulated by the FDA?

Yes, herbal supplements are regulated by the Food and Drug Administration, but not in the same way drugs are. Instead, they’re considered dietary supplements — that means manufacturers don’t have to seek FDA approval before selling dietary supplements.
Companies can claim that their herbal supplements address a nutrient deficiency, support health, or are linked to body functions — if they have supporting research and they include a disclaimer that the FDA hasn’t evaluated the claim. But they aren’t allowed to make a specific medical claim such as that the herb “treats” or “cures” a medical condition.
The manufacturers themselves are responsible for following safety and quality standards, but the FDA does monitor dietary supplements that are currently on the market. If it finds a product to be unsafe, it can take legal action.
How Can I Tell if a Supplement Is Good Quality?

Supplements require way less information on their labels than drugs do, and for good reason — they’re way less toxic. But the more information a company puts on the label, the better, says Dr. Rawls.
“Transparency is key to earning your trust. The label should clearly state which ingredients are in the supplement and the quantity of each, so you know what you’re putting into your body,” he says.
Ideally, you also want to know where those ingredients came from and how they were produced, Dr. Rawls says. That information should be on the label and/or the company’s website, along with their standards for ingredient quality, potency, and purity.
A few more ways to suss out reputable companies: Look to see whether a supplement carries the Good Manufacturing Practices (GMP) seal, indicating it was made in a facility that follows FDA regulations. And check whether it has been sent to a third-party lab, like U.S. Pharmacopeia, ConsumerLab.com, or NSF International, for independent verification of ingredient purity and label claims.
Does Insurance Cover Alternative Medicine?

Yes and no. Certain insurance companies are starting to cover some alternative treatments, like acupuncture, chiropractic therapy, and massage. But since there’s no across-the-board coverage, you should contact your insurance company directly to find out what your plan covers.
There are a few other ways to save on herbal therapy. If your employee offers a flexible spending account, you can use that to set aside pre-tax dollars (generally, each pay period) for health-related expenses; that money can then be used for herbal supplements and other alternative treatments. Similarly, a health savings account lets you set aside money on a pre-tax basis to pay for qualified medical expenses, but you would set this kind of account up yourself, not your employer.
We hope the list above addressed all of your questions about herbal therapy, but if not, don’t stop here! Keep doing your research: explore the VitalPlan.com blog or other trusted resources, or take your questions to an integrative health practitioner — just don’t let a lack of information stop you from gaining the many impressive health benefits of herbs.
Looking for More Wellness Tips?
Join our newsletter for bi-weekly tools, education, and savings to boost your health.
References
1. https://www.mayoclinic.org/drugs-supplements-st-johns-wort/art-20362212
_______________________
**Comment**
As always, I appreciate information provided by experienced doctors on any and all treatments for tick-borne illness, that said, please remember Dr. Rawls is in the business of selling an herbal treatment for Lyme/MSIDS.
Also, herbalists have differing opinions on what type of herb form is best. From what I’ve read and gathered, Master Herbalist Stephen Buhner, a highly respected herbalist who has helped countless patients, believes the whole herb is best due to the way it works synergistically. I’ve heard other herbalists state the same thing.
Tinctures and extracts can be very expensive. One of the cheapest herbal treatments is getting the whole, ground herb. Buhner’s books give excellent suggestions for dosage, sources, and many other details. I highly recommend his books.
My husband and I have used everything under the sun for treatment, with variable results. To be honest, we rarely if ever herxed on herbs – although we took plenty. We always herxed on antibiotics and had near immediate results. This was my standard if a treatment was working or not. Often out of desperation we did both herbs and antibiotics. I’m not saying herbs didn’t help or play a role – only that I didn’t physically notice any effects, and when you are forking out thousands of dollars on treatment, we have to make tough choices. It seems logical to me to choose the ones that are actively making a difference.
Anyone with this understands the desire to get well and the subsequent willingness to stick a needle in your eye if you thought for a second it might work! This desperation leaves patients vulnerable to quackery and ineffective treatments. This is why I believe it’s extremely important to have a Lyme-literate doctor helping you sift through fact vs fiction. Sometimes you need numerous doctors! After all, it’s impossible to know everything and each patient presents completely differently.
On a final note: I rejoice with all patients who have success with treatments – even if I wouldn’t use them myself or question their effectiveness. There’s much that is unknown about the effect of treatments upon the human body – as well as the synergistic effects of various treatments. On the other hand, I commiserate with patients who are struggling with treatments. Antibiotics, although effective for many, are extremely harsh on the body. This is a fact, and I understand patients’ fears and reluctance to use them. Personally, I hadn’t used antibiotics in over 20 years before I become infected with Lyme/MSIDS. I would try ANYTHING before taking antibiotics and it usually worked – or my body handled it on its own. But, getting tick-borne illness changed everything for us, forcing me to rethink my thoughts on them.
Healing is a powerful, complicated process. One that I don’t claim to understand in its entirety. We must remain open-minded but vigilant, making sure we are making forward progress (which sometimes means going backwards to go forwards!). In the end we must all make tough choices. I want to stand with you regardless of what treatment you choose. I will never vilify someone’s treatment – I may respectfully question it out of concern, but in the end it’s your choice and your healing. I’m here for everyone.

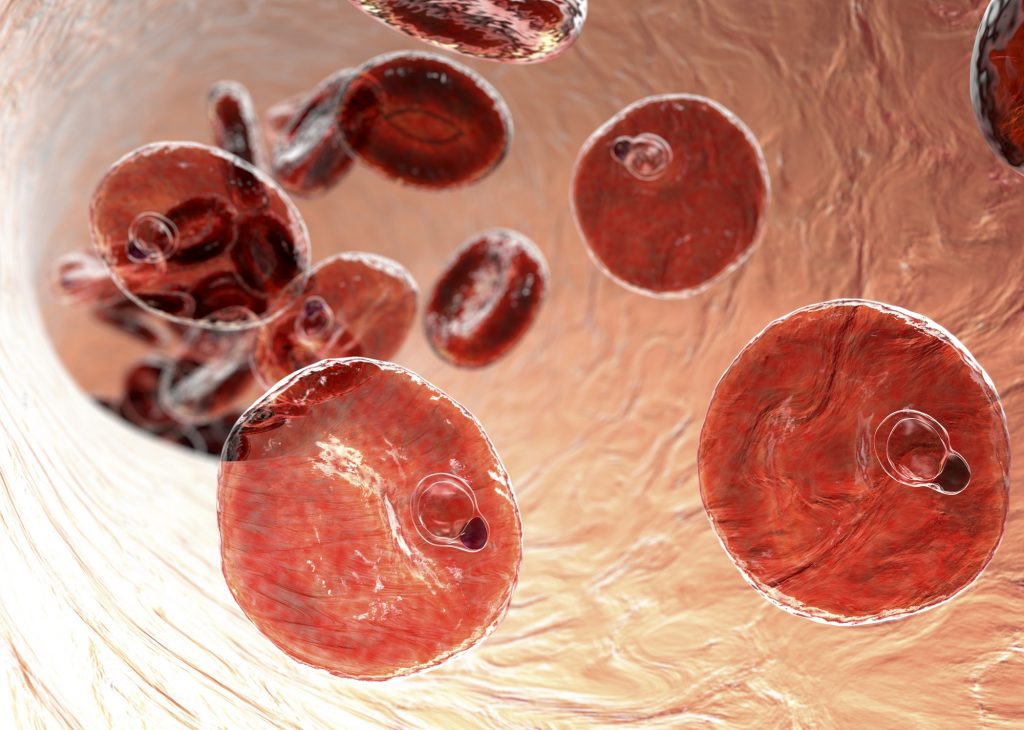
![[Real Talk] New Johns Hopkins Study: 5 Herbs that Can Kill Babesia](https://rawlsmd.com/wp-content/uploads/2021/04/Real-Talk-New-Johns-Hopkins-Study-5-Herbs-that-Can-Kill-Babesia.png)