Tick Bite Leads to Multiple Co-infections
https://danielcameronmd.com/tick-bite-multiple-co-infections/
Tick bite leads to multiple co-infections

In their case report “One man, three tick-borne illnesses” Grant and colleagues describe a 70-year-old man who was admitted to the emergency department with ongoing fevers, ankle edema and nausea. [1] One month earlier he noticed a small raised red lesion on his left ankle, which he believed was an insect bite.
“Two days after noting this ankle lesion, the patient noticed an erythematous rash on his neck and chest,” the authors explain. He was prescribed an antihistamine and 7-day course of trimethoprim–sulfamethoxazole.
The rash resolved after 5 days of antibiotic treatment, but the man continued to have pain and swelling in his ankle. The pain spread to his left hip and he was “diagnosed with sciatica and prescribed gabapentin.”
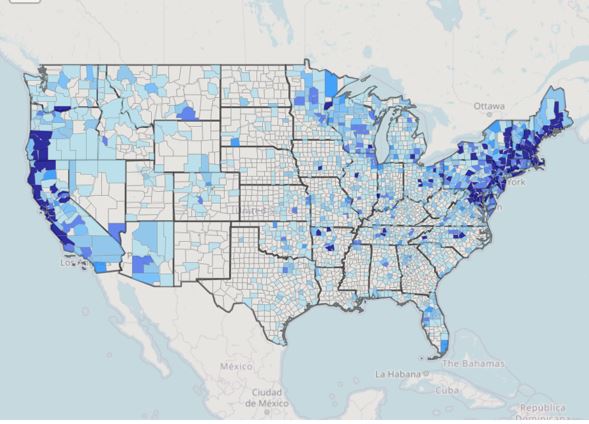
The patient had reportedly travelled to an endemic area of the United States. And was therefore, suspected of having a tick-borne illness.
“Physicians must maintain a high level of suspicion for co-infection, as untreated disease can result in long term and sometimes life-threatening sequelae,” the authors suggest.
He tested positive for Borrelia burgdorferi, Anaplasma phagocytophilum and Babesia microti serologies.
The patient’s symptoms improved with treatment, but one year later, he continued to have symptoms of neuropathy at the site of the presumed insect bite.
References:
- Grant L, Mohamedy I, Loertscher L. One man, three tick-borne illnesses. BMJ Case Rep. 2021 Apr 16;14(4):e241004. doi: 10.1136/bcr-2020-241004. PMID: 33863772; PMCID: PMC8055128.
__________________
**Comment**
A perfect example of how mainstream medicine is hopelessly lost in its own hubris.
- Seven days of treatment of anything will not solve this
- trimethoprim–sulfamethoxazole, commonly known as Bactrim DS will not touch Babesia at all
- Bactrim DS, while a great drug, should not be the first choice for Lyme disease – and he had a clear EM rash, which is diagnostic for Lyme – no testing required
- It is common knowledge that the EM rash will wax and wane all on its own and should never be used to determine if treatment is working or not
- Doxycycline is still the best front-line drug for both Lyme and Anaplasmosis, but is far from sufficient in and of itself
- It is not surprising at all that this poor man continued to suffer with neuropathy, which they will undoubtedly blame on anything but tick-borne illness and it will never occur to them in a million years to treat him with numerous antimicrobials simultaneously for far longer than 7 days. Myopia is a a very real condition
For more:
- https://madisonarealymesupportgroup.com/2021/09/30/single-tick-bite-leads-to-3-diseases-in-elderly-woman/
- https://madisonarealymesupportgroup.com/2017/07/01/one-tick-bite-could-put-you-at-risk-for-at-least-6-different-diseases/ (It’s actually 19 and counting diseases)
- https://madisonarealymesupportgroup.com/2021/07/13/lyme-coinfection-comparisons-what-your-symptoms-could-be-telling-you/
- https://madisonarealymesupportgroup.com/2018/10/30/study-shows-lyme-msids-patients-infected-with-many-pathogens-and-explains-why-we-are-so-sick/
- https://madisonarealymesupportgroup.com/2021/08/31/the-added-battle-for-lyme-patients-coinfections/
- https://madisonarealymesupportgroup.com/2015/12/14/closing-in-on-the-8/ My guess is it’s far greater than 8%
For Lyme treatment: https://madisonarealymesupportgroup.com/2016/02/13/lyme-disease-treatment/
For Anaplasmosis treatment: https://madisonarealymesupportgroup.com/category/anaplasmosis-treatment/
For Babesia Treatment: https://madisonarealymesupportgroup.com/category/babesia-treatment/