Complaint Against Dr. Paul Gisbert Auwaerter License Number: D0041413
Complaint against Dr. Paul Gisbert Auwaerter License Number: D0041413

Please see the following complaint submitted to the Maryland Board of Physicians along with their response. I followed up in disgust as the disinformation continues year after year decade after decade by the same deceitful individuals who have been propagating the false Lyme disease narrative.
If you agree with my complaint, please voice your concerns by writing to Wes Moore, Governor of Maryland where Dr Paul Auwaerter practices medicine. Reference this Petition Update link and lets flood his inbox with emails! (No matter where you live!!)
governor.mail@maryland.gov
lt.governor@maryland.gov
Picture of Governor Moore found here: https://www.mbp.state.md.us/
———- Original Message ———-
From: CARL TUTTLE <runagain@comcast.net>
To: “mdh.mbp_intake@maryland.gov” <mdh.mbp_intake@maryland.gov>
Cc: “oag@oag.state.md.us” <oag@oag.state.md.us>, “cquattrocki@oag.state.md.us” <cquattrocki@oag.state.md.us>, “musa.eubanks@oag.state.md.us” <musa.eubanks@oag.state.md.us>
Date: 06/21/2025 7:56 AM EDT
Subject: Complaint against Dr. Paul Gisbert Auwaerter License Number: D0041413
June 21, 2025
Maryland Board of Physicians
Complaint Intake Unit
4201 Patterson Avenue
Baltimore, MD 21215
Re: Dr. Paul Gisbert Auwaerter, License Number: D0041413
To whom it may concern,
I would like to file a complaint against Dr. Paul Gisbert Auwaerter for propagating false/misleading statements regarding the testing and treatment of tick-borne diseases as there exists a substantial risk of serious harm to public health, safety, and welfare from his misinformation.
Please see the following correspondence with Dr Auwaerter and Medscape’s Editorial Staff regarding the misinformation Auwaerter has been allowed to spread (and viewed by physicians across the country) essentially downplaying the threat of tick-borne disease co-infections while claiming serology for Lyme disease is a “good test.” This deliberate misrepresentation is an ethical concern as Auwaerter, past president of the Infectious Diseases Society of America, is considered an “expert” in the field.
This is not an isolated case. The IDSA has had a history of misinformation; In 2021, the Patient Centered Care Advocacy Group demanded the removal of an inaccurate statement by the IDSA which excluded maternal-fetal transmission of Lyme disease. Congenital transmission was fist described in 1985.
Advocate asks IDSA to remove false statement about Lyme transmission
https://www.lymedisease.org/fries-idsa-remove-false-statements/
Auwaerter was the lead author of the deplorable Lancet Infectious Disease article:
Antiscience and ethical concerns associated with advocacy of Lyme disease
https://pubmed.ncbi.nlm.nih.gov/21867956/
Please consider sending a cease-and-desist letter to Dr. Auwaerter demanding an end to his engaging in this harmful misinformation campaign and require a correction and/or retraction of the statements identified in the correspondence that follows.
A response to this complaint is requested.
Respectfully submitted,
Carl Tuttle
Independent Researcher
Hudson, NH
Cc: Anthony G. Brown, Attorney General
Carolyn A. Quattrocki, Chief Deputy Attorney General
Musa L. Eubanks, Principal Counsel Maryland Department of Health
Correspondence with Dr Auwaerter and Medscape’s Editorial Staff:
———- Original Message ———-
From: CARL TUTTLE <runagain@comcast.net>
To: “pauwaert@jhmi.edu” <pauwaert@jhmi.edu>, “pgauwaerter@gmail.com” <pgauwaerter@gmail.com>
Cc: “aaguilar@webmd.net” <aaguilar@webmd.net>, “DFlapan@Medscape.net” <DFlapan@Medscape.net>, “lkane@medscape.net” <lkane@medscape.net>, “gamiller@medscape.net” <gamiller@medscape.net>, “dolmos@webmd.net” <dolmos@webmd.net>, “sarah.wright@webmd.net” <sarah.wright@webmd.net>, “editor2@webmd.net” <editor2@webmd.net>, “mmcnutt@nas.edu” <mmcnutt@nas.edu>, “jliao@nas.edu” <jliao@nas.edu>, “news@medscape.net” <news@medscape.net>
Date: 06/15/2025 12:13 PM EDT
Subject: Medscape: Chronic Lyme Infection-Associated Illness in Urgent Need of Symptom-Targeted Treatments
June 15, 2025
The IDSA Foundation
1300 Wilson Boulevard Suite 300
Arlington, VA 22209
Attn: Paul Auwaerter, vice chair of the IDSA Foundation
Dr Auwaerter,
I would like to call attention to the following Medscape article referencing the recent National Academies of Sciences review of Lyme disease through a recommendation of the Tick Borne Disease Working Group calling for a review of all the literature.
Medscape Medical News June 10, 2025
Chronic Lyme Infection-Associated Illness in Urgent Need of Symptom-Targeted Treatments
https://www.medscape.com/viewarticle/chronic-lyme-infection-associated-illness-urgent-need-2025a1000fhv
Regarding laboratory testing…
“The current two-tier serologic testing approach based on the Dearborn criteria has limitations and may not detect all cases of Lyme disease, particularly in patients with early or late disease or those who remain symptomatic after treatment.”
In contrast Dr. Auwaerter you continue to promote serology as a “Good Test” with your recent recorded interview for the so-called “Clinician Toolkit” promoted by the American Medical Association which just so happened to be paid five million dollars to buy into this misinformation through CDC grant# NU50CK000597
Oct 3, 2024
Improving Care for Patients with Prolonged Symptoms and Concerns about Lyme Disease: A Clinician Toolkit
https://www.ama-assn.org/delivering-care/public-health/improving-care-patients-prolonged-symptoms-and-concerns-about-lyme
Imbedded recording:
Understanding Lyme Disease with Dr. Paul Auwaerter (@12:30 into the recording)
“If you have symptoms for more than a few weeks it’s a very good test and I think there’s a common misconception it’s not a good test. And what is true is it’s not a good test if you’ve only been infected for a week or two because the body hasn’t mounted enough time to develop antibodies. But if people have had symptoms for three, four weeks or longer, it is a good blood test to help assess these later symptoms that could be neurologic, muscular, skeletal, or occasionally cardiac.” – Paul Auwaerter
Serology is so unreliable that in 2013 Virginia Governor Bob McDonnell signed HB1933 into law requiring healthcare providers to notify those tested that current laboratory testing can produce false negatives.
Governor Chris Sununu’s 2020-2021 commission to study diagnostic testing for Lyme disease concluded that the FDA approved two-tier serologic immunoassay for Lyme was not reliable in all stages of disease; no better than a coin toss.
Peer-reviewed evidence of “Seronegativity in Lyme borreliosis and Other Spirochetal Infections” 16 September 2003
https://www.dropbox.com/s/3d6m45jzlhhwalu/Seronegativity.pdf?dl=0
And yet Dr. Auwaerter you continue to promote serology as a “good test”
Furthermore, you refused to answer my inquiry regarding your Medscape commentary of Oct 2023
Medscape COMMENTARY
New Federal Oversight of Lab Developed Tests
https://www.medscape.com/viewarticle/997365
Excerpt:
“I often see patients who are concerned they might have Lyme disease, or they’ve been told by other physicians that they have a tickborne or multiple infections. I’ve had patients who claim to have five or six infections: Lyme disease, Babesia, Bartonella, Mycoplasma, or Epstein-Barr virus. They bring LDT results from outside laboratories, which often have a proviso that these tests are only for research or educational purposes. Yet, they purport finding analytes (antibodies or proteins) that suggest the patient has an active infection. These patients may have been treated but are not improving, so they are referred to me.” – Paul Auwaerter
Carl Tuttle’s Inquiry: (which remains unanswered and posted to that commentary)
Dr. Auwaerter… I would like to call attention to the following 2009 tick study conducted here in New Hampshire:
Correlation between Tick Density and Pathogen Endemicity, New Hampshire
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2671416/
The study found deer ticks were carrying multiple pathogens (co-infections) that could be transmitted in a single bite.
What FDA approved Tick-Borne Disease Panel are you recommending so as not to miss any of these infections?
A response to this inquiry is requested.
Carl Tuttle
Hudson, NH
___________________
Dr. Auwaerter,
Are you aware of the following announcement? IGeneX is finding those “multiple infections” you claim do not exist….
IGeneX Lyme ImmunoBlot test kit receives FDA clearance
https://www.lymedisease.org/lyme-immunoblot-fda-clearance/
GETTING STARTED WITH IGENEX
https://igenex.com/wp-content/uploads/getting-started-with-igenex.pdf
A 2018 study of 10,000+ patient samples from nearly every state:
37.3% were positive for Babesia species
32.1% for Lyme Borrelia
27.7% for TBRF Borrelia
19.1% for Bartonella
16.7% for Anaplasma
12.8% for Rickettsia
6.9% for Ehrlichia
Co-infections:
40% tested positive for two pathogens
15% tested positive for three pathogens
4.6% tested positive for four pathogens
0.7% tested positive for five pathogens
What is going on here Dr. Auwaerter? Are you completely uninformed or deliberately promoting misinformation? Will you be correcting/retracting your statements?
A response to this inquiry is requested.
Carl Tuttle
Independent Researcher
Hudson, NH
Cc: MEDSCAPE EDITORIAL STAFF
Marcia McNutt, President of the National Academy of Sciences and Chair of the National Research Council
Send comments and news tips to news@medscape.net
_________________________________________________________________
To the Maryland Board of Physicians:
Additional complaints against Auwaerter:
1. The Mayday Project Responds to Dr. Paul Auwaerter’s Defense of IDSA Guidelines for Lyme Disease
https://www.webwire.com/ViewPressRel.asp?aId=192558
2. Hopkins Physician Says Lyme Disease Patients Create Conspiracy Theories About Their Illnesses
https://www.webwire.com/ViewPressRel.asp?aId=197392
3. Mothers Against Lyme Calls for Retraction of False Information on Congenital Lyme in IDSA, AAN, ACR Guidelines
Retraction request cites harm to pregnant women and children
https://www.webwire.com/ViewPressRel.asp?aId=281005
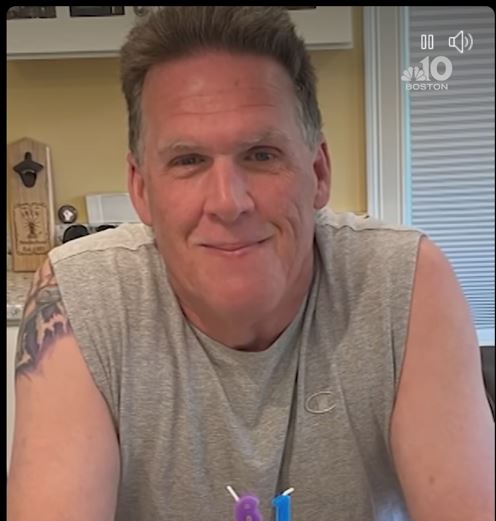
4. Detailed patient experience because of the false information (Please read)
https://www.facebook.com/photo/?fbid=30451510191160844
Excerpt:
“I’ve tried explaining this a few times and I won’t stop until people get it. This isn’t like cancer or any other disease where I can go to a Dr that’s covered by my insurance and receive treatment. What is happening here is criminal and if you don’t believe me, ask ANYONE with Lyme.”
Response from the Maryland State Board of Physicians
———- Original Message ———-
From: MDH mbp_intake -MDH- <mdh.mbp_intake@maryland.gov>
To: CARL TUTTLE <runagain@comcast.net>
Date: 06/26/2025 11:09 AM EDT
Subject: Re: Complaint against Dr. Paul Gisbert Auwaerter License Number: D0041413
Good morning, Mr. Tuttle:
Thank you,
Intake Unit
Maryland State Board of Physicians
The Board of Physicians is committed to customer service. Please visit https://www.doit.state.md.us/selectsurvey/TakeSurvey.aspx?agencycode=MBP&SurveyID=86M2956 to take our Customer Satisfaction Survey.
My reply to the Maryland State Board of Physicians:
———- Original Message ———-
From: CARL TUTTLE <runagain@comcast.net>
To: MDH mbp_intake -MDH- <mdh.mbp_intake@maryland.gov>, “jennifer.saylor-florio@maryland.gov” <jennifer.saylor-florio@maryland.gov>
Cc: “Harbhajan.Ajrawat@maryland.gov” <Harbhajan.Ajrawat@maryland.gov>, “Christine.Farrelly@maryland.gov” <Christine.Farrelly@maryland.gov>, “hajrawat@gmail.com” <hajrawat@gmail.com>, “oag@oag.state.md.us” <oag@oag.state.md.us>, “cquattrocki@oag.state.md.us” <cquattrocki@oag.state.md.us>, “governor.mail@maryland.gov” <governor.mail@maryland.gov>, “lt.governor@maryland.gov” <lt.governor@maryland.gov>
Date: 06/27/2025 8:31 AM EDT
Subject: Re: Complaint against Dr. Paul Gisbert Auwaerter License Number: D0041413
Intake Unit
Maryland State Board of Physicians,
via <jennifer.saylor-florio@maryland.gov>
Dr. Saylor-Florio,
I would like to call attention to the following statement found in the attached response to my complaint against Dr Paul Auwaerter:
“The Board of Physicians is responsible for assuring that licensed physicians and allied health practitioners render competent medical care to the citizens of Maryland”
Isn’t that statement a bit hypocritical when you allow a physician to claim serology for Lyme disease is a “good test” when in fact it is no better than a coin toss while using his position of authority as past president of the IDSA to propagate that falsehood?
I question the credibility of this medical board willing to turn a blind eye to Auwaerter’s misleading statements. How could he possibly provide competent medical care believing that serology is a good test while tick-borne co-infections are of little concern? The potential for harm or negative outcomes is substantial and noteworthy.
Carl Tuttle
Independent researcher
Hudson, NH
Cc: Harbhajan Ajrawat, M.D. Chair
Anthony G. Brown, Attorney General
Carolyn A. Quattrocki, Chief Deputy Attorney General
Wes Moore, Governor
Aruna Miller Lt Governor
_______________
**Comment**
I find it quite telling that the Maryland Board of Physicians claims it does not have legal authority to investigate Dr. Auwaerter’s patently false statements about Lyme testing. State Boards over Physicians had no trouble whatsoever investigating and persecuting any doctor during COVID who advocated for treatments (ivermectin, HCQ, vitamins, etc.) other than what the top-down accepted narrative had to offer (ventilators, remdesivir, the clot shot, etc), or whom questioned the clot shot gene therapy which was touted as ‘safe and effective,” like a mantra.
Do not expect justice from these ‘professional’ medical groups.
They are on the wrong side of the fence.
For More:
- https://madisonarealymesupportgroup.com/2020/09/25/why-should-we-care-about-lyme-disease-a-colorful-tale-of-government-conflicts-of-interest-probable-bioweaponization-and-pathogen-complexity/
- https://madisonarealymesupportgroup.com/2019/02/22/why-mainstream-lyme-msids-research-remains-in-the-dark-ages/
- https://madisonarealymesupportgroup.com/2020/03/11/cdcs-recommendations-for-lyme-epitomize-institutional-bias/
- https://madisonarealymesupportgroup.com/2018/02/11/anti-patient-bias-embedded-in-tickborne-disease-working-group-and-its-subcommittees/
- https://madisonarealymesupportgroup.com/2022/10/28/lyme-advocate-asks-tbdwg-where-we-are-today-after-a-6-year-pacifier-answer-no-where/