Listen Here:
Read the transcript below
In this interview you’ll learn more about a complication of Lyme disease known as Lyme carditis.
Interview condensed for clarity and length
My name is Lindsy Swift, Director of Marketing and Communications at Global Lyme Alliance. And I am pleased to be speaking with Dr. Baranchuk today on a very important topic that needs more education and awareness. Welcome, Dr. Baranchuk.
Dr. Baranchuk is one of the world’s leading experts on Lyme carditis. He is a Professor of Medicine at Queen’s University in the Division of Cardiology in Ontario, Canada. Dr. Baranchuk is also editor-in-chief of the Journal of Electro Cardiology, International Society of Holter and Non-invasive Electrocardiology, and President-Elect of the Interamerican Society of Cardiology. Dr. Baranchuk has published more than 750 articles in well-recognized international journals, 67 book chapters, and has presented more than 260 abstracts around the world. So for the purpose of this interview today, Dr. Baranchuk, let’s start off with a review of Lyme carditis. An easy question:
What is Lyme Carditis?
Dr. Adrian Baranchuk:
Thank you very much, Ms. Swift. As I said, it’s a pleasure to have the opportunity to chat about Lyme carditis with you today. So basically, most of our audience is familiarized with Lyme disease. So you got a tick bite, all of the sudden there is the dermatological manifestation. Sometimes it is the classic, we call it erythema migrans, which is that target lesion. But we know now that dermatological manifestation can vary and be something less common. And then the patient usually develops fever and what we call constitutional symptoms, which are those specific symptoms of not feeling well, feeling extremely weak, sometimes joint pain. And then this is what motivates going to the consult.
And when the skin manifestation is very obvious, then Lyme disease is first on the list. Or if these things happen in regions where doctors are aware that Lyme disease is very prevalent, we call it endemic regions, right? For example, my city, Kingston in Ontario, Canada, it’s a well-known zone for Lyme disease. So when patients come with these vague symptoms, somebody will suspect and send a serology to do the diagnosis. But your question specifically is how do we go from this skin manifestation to a heart lesion that we call Lyme carditis?
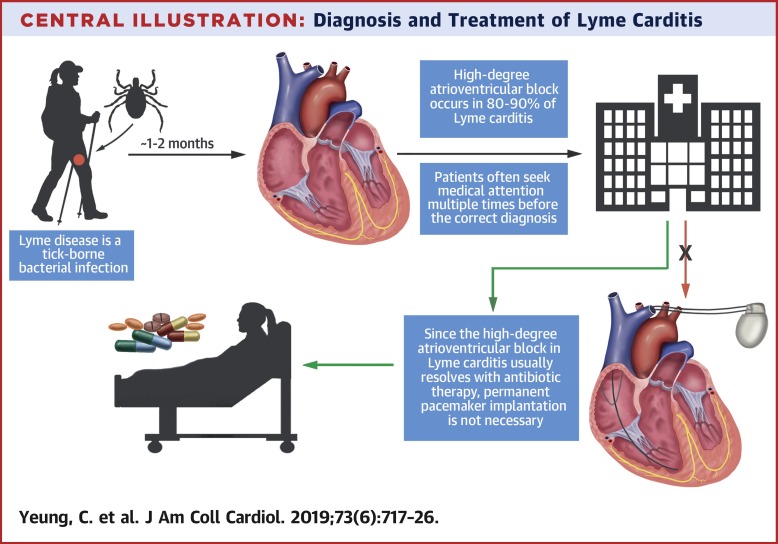
Well, it happens that the bacteria through the skin can enter the bloodstream, and then it’s distributed to many different parts in the body. And depending where the bacteria lands is where you are going to have your more classic manifestations. If it goes to the joints, is when you are going to have early disseminated Lyme arthritis. If it goes to your brain, you will have the early disseminated neuroborreliosis. I know it’s a tough name, but when the bacteria lands in your brain, sometimes what it happens is that it lands in your heart.
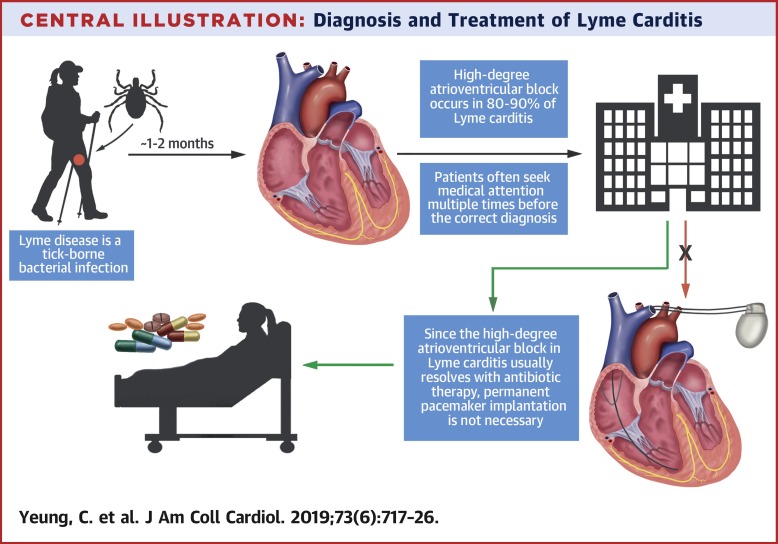
And then we call it Lyme carditis. Lyme carditis, as you said, occurs when the Lyme bacteria, the so-called Borrelia, affects your heart tissue. And for some reason, this bacteria has a special appetite for the electricity of your heart. It lands nine over ten times over your conduction system, which helps the heart contracting. And what it does is that it can slow down those contractions sometimes to the point that the heart stop beating. And if you are not resuscitated, this could be fatal. The other 10% of the time, it affects the muscle and the tissue that covers the heart. And we call that myopericarditis.
“…we should do ECGs to every single individual where you suspect or confirm Lyme disease…”
So, how often this happens, if you go to the literature, and I want your audience to pay attention to because this is something that is coming out in our research for the next two years. If you go to the literature, you will find that the heart is involved in Lyme disease 4 to 10% of the time. But Lindsy, this happens when the patient has symptoms.
So, during the description to the doctors, they say, and in addition of fever, this rash, my pain in the joints, I almost lost consciousness two times. Or I’m having chest pain or I’m having shortness of breath. And all of the sudden the doctor of decides to put one ECG and auscultation of your heart in the combo of your care for Lyme disease. And this is how we arrive to four to 10%, meaning this is not the real number. For the real number, we should do ECGs to every single individual where you suspect or confirm Lyme disease and put your stethoscope that machine we use to listen to your heart, in every single patient that you suspect or confirm Lyme disease. And my perception is that number could go much higher than 10%.
Dr. Adrian Baranchuk:
But you will say why? How do you know Adrian, that that is possible?
Dr. Adrian Baranchuk:
Two reasons. One reason is that we have seen cases where patients are completely asymptomatic, they don’t feel anything on their heart, but the doctor was wise enough to include one ECG and we see manifestations of Lyme carditis there.
Dr. Adrian Baranchuk:
And the second is that the group in Philadelphia basically looking at young kids with Lyme disease, they decided to do this systematic search. And you know what, Lindsy? The prevalence of heart complications increased to 27%.
Lindsy Swift:
That’s scary.
Dr. Adrian Baranchuk:
So, what we want is to run studies on every single current study that is being done in the world about Lyme disease to include two simple cheap things. A $1 ECG, and a half of a dollar auscultation of the heart. And you may say, well, interim, but if they are diagnosed with Lyme disease, they are going to be treated so that may treat all Lyme disease and the heart, true. However, the type of antibiotic that you use, the administration way for the antibiotic to reach the patient, and the duration of the antibiotic treatment differs if you only have Lyme disease or if you have a Lyme carditis.
Lindsy Swift:
Right. So, this should be something that doctors should be doing when they suspect Lyme disease every time, is what you’re saying?
Dr. Adrian Baranchuk:
Every time. But for me, Lindsy, to say it with the same degree of confidence that you have said that, and I know I’m going to remove my clinical hat to put on my research hat, is I need research to prove that your observation, my observation, and the observation of plenty of clinicians and investigators around the world is true so we can systematically include the 12-lead ECG, I insist. Five minutes to obtain, $1, highly reproducible, easy to be transmitted by phone. So I can’t foresee family doctors working in remote areas where Lyme disease could be prevalent doing an ECG in their office and transmitted this ECG to a colleague of their confidence saying, I just got this ECG. Can you confirm if it’s normal or not? Because if it is abnormal, the patient may need to be transferred from where the patient is located to a center that can do cardiac monitoring.
Dr. Adrian Baranchuk:
So, I would love to demonstrate this. When you interview me in, let’s say 2025, again, I can tell you, do you remember that conversation, Lindsy? We were right.
Lindsy Swift:
Right.
Dr. Adrian Baranchuk:
Because now we increase the prevalence of Lyme carditis from 10% to, I don’t know, 22, 25%.
Lindsy Swift:
Are there any plans in your research or anyone you know that’s doing this research out there that’s going to start doing this so that we have those numbers?
Dr. Adrian Baranchuk:
So first, my recognition to Dr. Beech, she was one if, I can’t recall if it was the lead author, but she’s one of the authors down in, I say down because I am in Canada, a little bit higher than that. By the way, let me brag a little bit because a book is coming called Lyme Carditis from A to Z, and it’s going to be printed by Springer, we hope, mid-2023.
Lindsy Swift:
Oh, great.
Dr. Adrian Baranchuk:
And this group has written the chapter on Lyme carditis in kids and young teenagers. A fantastic group, they work very hard and they were leading this idea. So, now we have conversations with different groups that have ongoing research to see if we can do a sub study. But at the same time, we are designing an observational project that could insert ECG as part of the mandatory test to do in every person diagnosed or highly suspected.
Remember that in some parts of the world, like in Canada, when we suspect Lyme disease, the serology takes five to seven days to return. So, if I truly suspect Lyme disease and there is an ECG with an abnormality, rather than sending the patient home on antibiotics for mouth, these patients should be admitted for IV antibiotics. And the question should be why? Because we have demonstrated more than five years ago that the progression of Lyme carditis can take from minutes to hours to days. So if I see a minor affection of the conduction system, this can be transformed into an emergency in a matter of hours. So if I’ve been lucky enough to have a minor thing, it corresponds to admit the patient, monitor the heart and start IV antibiotics until we receive the results of this serology.
…But we do know, and we have published, that unrecognized Lyme carditis can lead to death. And that can happen in a matter of minutes, hours or days. But please, to all the healthcare providers, if you are suspecting or diagnosing Lyme disease, make your effort to rule out whether the heart is being involved or not.
Does diagnosing Lyme in Lyme carditis differ in pediatric versus adult patients?
Dr. Adrian Baranchuk:
This is an excellent question. So, the older the patient, you may have conditions that produce some heart impact that are independent on whether you have Lyme disease or not. And I do receive, and I see patients from all around the world that they come to Kingston for a 30-minute interview. For me to say, it is impossible to determine today if the symptoms that you have have anything to do with your Lyme disease that you suffered three years ago or not. And I’m very sad because if you are 65, 70, 75, having cardiovascular symptoms is extremely common. It’s more common than COVID, right? Cardiovascular diseases are the main cause of symptoms in patients older than 65 years of age. So, in order for me to connect that to Lyme, sometimes it’s difficult.
It’s easier when I receive emails from centers saying a patient has come with this ECG and this and this and this symptom. Do you think that the patient could have Lyme carditis? And for that, in 2018, so five years ago, we have published the SILC score. SILC, S-I-L-C, which stands for Suspected Index in Lyme Carditis, and it uses an acronym invented by one of my fellows at the time, Dr. Juan, that is called COSTAR. The COSTAR is constitutional symptoms, outdoor activities for the O. Sex, male seems to be more prevalent than female, something that needs further investigation, but so far is a three to one relationship.
Dr. Adrian Baranchuk:
Recognition of a tick bite, not every person recognizes that. But if I have symptoms and abnormal ECG and a guy that says, “Oh, three weeks ago I removed, I went for a hike and I removed a tick from my leg or from my groin.” Well, here it is. Age, so this is a disease that affects younger individuals, so age less than 50. And R for rash. If you tell me I do, I did have a rash, now it dissipated. When you have more than seven points to 12 for a total of 12, the possibility of that condition being Lyme carditis is so high that even without the serology, you should be admitted, take blood for serology, start the antibiotic. Three to six is intermediate, so we advocate for patients to be admitted anyway and telling them we’re going to treat you until we get the serology back.
Now, zero to two points is unlikely. So unlikely to be Lyme disease that if you even don’t want to ask for serology, you’re okay with that, just proceed and put a pacemaker on the patient. So I am super happy to tell you that since we published this in 2019, several groups from different parts of the world have been using it with a very high sensitivity. For your audience, that means that it’s very useful. So it helps a lot when you have an abnormal ECG and some of the symptoms that we’ve been describing for you to run the SILC score, use the COSTAR acronym, and if you have an intermediate to high mark, then to be admitted in hospital, don’t allow those patients to go home because then it happens the catastrophes that we’ve been discussing earlier.
Treatment for Lyme Carditis
Lindsy Swift: So you mentioned earlier that the treatment for it is IV antibiotics. Is that correct?
Dr. Adrian Baranchuk:
That is correct. The proposed use of antibiotics is for 10 to 14 days of IV antibiotics depending on the response. It happened to us several cases that by day five, they recover conduction. If the patient require a temp perm, we remove it. By day seven, we put them on the treadmill. Treadmill, they exercise 150, 160 beats per minute. We send them home and we shift to doxycycline to complete a total of three weeks of antibiotic treatment.
Dr. Adrian Baranchuk:
So the IV is until you recover the conduction. Then we switch to doxy at the time of the discharge, and the patient completes a total of three weeks. So let’s say that you’ve been one week on IV, you will take two more weeks. If you’ve been two weeks on IV, you will take only one week.
Lindsy Swift:
Okay. And is that that done in the hospital, or can it be in outpatient?
Dr. Adrian Baranchuk:
Well, if you are on IV antibiotics is because the suspicion of Lyme carditis is quite high and/or you have the confirmation already. So we propose that during the IV antibiotic with or without a temp perm because remember that there’s people that tolerates being at 40 beats per minute very well, and they don’t need the temp perm, but they need to be observed. Why? Because the progression from that to no cardiac beats can be very quick. Even if you’re treated on antibiotics, it happens that some patients may not respond to it. So while the patient is receiving IV antibiotics, we aim for the patients to be at the hospital. There are experiences in the US where the home care provided was excellent, and patients have received the IV antibiotic with a temp perm at home. And at the time of improvement, both things were removed, IV to PO complete three weeks, and removal of the device in the hospital. Here in Canada, we do not advocate to have patients with a temp perm connected to their heart at home. We prefer to keep an eye on them at all times.
Lindsy Swift:
Do you treat pediatric cases the same as adult cases? Is the treatment the same?
Dr. Adrian Baranchuk:
You do. If the kid is able to tolerate a severe bradycardia, but he’s asymptomatic, IV antibiotics, monitoring.
Dr. Adrian Baranchuk:
If the kid has collapsed, presented fainting, and a total interruption of their heart electricity, they get a temp perm (pacemaker).
Dr. Adrian Baranchuk:
Because we don’t want that kid, maybe with a perm to be walking the corridor, we don’t want that. If I put a regular temporary pacemaker, the patient has to be in bed 24/7. So, this new strategy allows the person to walk while waiting to improve. So at the time of improvement, boom, home. I want to tell you very briefly an experience that we published very recently.
Dr. Adrian Baranchuk:
Two patients in different centers. They got Lyme carditis suspected, they got this serology, they started the IV antibiotics, but in the centers, they decided to implant a permanent pacemaker. So, the patients were contacted and say, your Lyme test came positive, please receive three weeks of antibiotic treatment. Both patients, one male, one female, have followed this indication. And for some reasons, they came to see me within one year of having that pacemaker implanted. So we did all the testing, demonstrated that they were not using their pacemakers because they received proper antibiotic treatment for myocarditis. We explained the risks associated with the extraction of the pacemaker. We proceeded to implant pacemakers. These were done in February and April 2022. After one year, they are doing their normal life with no pacemakers so.
Dr. Adrian Baranchuk:
This is something to keep reflecting. We need more education within the healthcare system to avoid in the first case, to implant the pacemaker, the permanent pacemaker if it is not absolutely necessary.
Lindsy Swift:
Is there anything else that we didn’t go over that you feel like we need to discuss in regards to Lyme carditis?
Dr. Adrian Baranchuk:
No. Maybe saying that I do believe that research in the arena of determining how prevalent Lyme carditis is in patients with confirmed or highly suspected Lyme disease is still lacking. And the second thing is we need more educational platforms, books, webinars, conversations like this to help healthcare providers to have Lyme disease very high in their differential when patients come with conduction disorders at a young age. And for any patient that comes with conduction disorders living in an endemic region. So in regions where life, this is quite prevalent. So from that perspective, I only can thank you for the opportunity to keep spreading the voice along the world.
Lindsy Swift:
Well, thank you for your great work, and we’ll be sure to link your published articles and important articles that people should read in regards to Lyme carditis at the bottom of this interview. Thank you again for your time, and it was a great conversation.
Dr. Adrian Baranchuk:
Thank you so much, Ms. Swift, and I am at your disposal at any time.
For more: