Study Shows Lyme/MSIDS Patients Infected With Many Pathogens and Explains Why We Are So Sick
**UPDATE May 2022**
This important article was retracted in Feb. 2022 due to:
The main method utilised in this study is an ELISA assay. An investigation by the University of Jyväskylä, Finland, has concluded that the patient selection and description in this Article, and in an unpublished report validating the methods used, do not justify the results presented. The Editors therefore no longer have confidence in the results and conclusions presented in this Article.
Kunal Garg, Leena Meriläinen, Heidi Pirttinen, Marco Quevedo-Diaz, Stephen Croucher and Leona Gilbert disagree with this retraction. Ole Franz did not respond to correspondence from the Editors about this retraction.
I can only surmise that ‘the powers that be’ are not happy with the attention this work has gotten and therefore want to erase it from history.
https://www.nature.com/articles/s41598-018-34393-9?fbclid=IwAR3k-zPy2rJu8OuFl3HHqJ0twLPJvQrxiIUALUs0T-BuuJ50_1VQVwcflIQ (Please see comment at end of article)
Evaluating polymicrobial immune responses in patients suffering from tick-borne diseases
Kunal Garg, Leena Meriläinen, Ole Franz, Heidi Pirttinen, Marco Quevedo-Diaz, Stephen Croucher & Leona Gilbert
Scientific Reportsvolume 8, Article number: 15932 (2018) https://doi.org/10.1038/s41598-018-34393-9
Abstract
There is insufficient evidence to support screening of various tick-borne diseases (TBD) related microbes alongside Borrelia in patients suffering from TBD. To evaluate the involvement of multiple microbial immune responses in patients experiencing TBD we utilized enzyme-linked immunosorbent assay. Four hundred and thirty-two human serum samples organized into seven categories followed Centers for Disease Control and Prevention two-tier Lyme disease (LD) diagnosis guidelines and Infectious Disease Society of America guidelines for post-treatment Lyme disease syndrome. All patient categories were tested for their immunoglobulin M (IgM) and G (IgG) responses against 20 microbes associated with TBD. Our findings recognize that microbial infections in patients suffering from TBDs do not follow the one microbe, one disease Germ Theory as 65% of the TBD patients produce immune responses to various microbes. We have established a causal association between TBD patients and TBD associated co-infections and essential opportunistic microbes following Bradford Hill’s criteria. This study indicated an 85% probability that a randomly selected TBD patient will respond to Borrelia and other related TBD microbes rather than to Borrelia alone.
A paradigm shift is required in current healthcare policies to diagnose TBD so that patients can get tested and treated even for opportunistic infections.
Please see link for full article. Snippets below:
Introduction
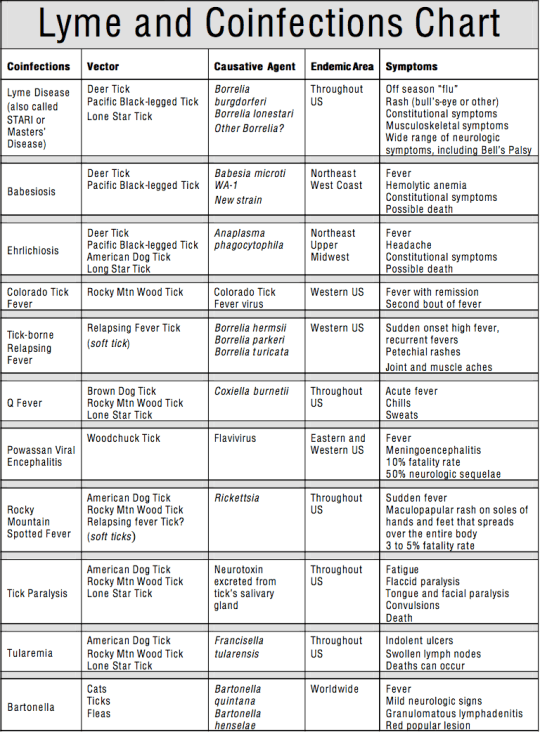
Tick-borne diseases (TBDs) have become a global public health challenge and will affect over 35% of the global population by 20501. The most common tick-borne bacteria are from the Borrelia burgdorferi sensu lato (s.l.) group. However, ticks can also transmit co-infections like Babesia spp.2, Bartonella spp.3, Brucella spp.4,5,6,7,8, Ehrlichia spp.9, Rickettsia spp.10,11, and tick-borne encephalitis virus12,13,14. In Europe and North America, 4–60% of patients with Lyme disease (LD) were co-infected with Babesia, Anaplasma, or Rickettsia11,15,16. Evidence from mouse and human studies indicate that pathogenesis by various tick-borne associated microbes15,16,17 may cause immune dysfunction and alter, enhance the severity, or suppress the course of infection due to the increased microbial burden18,19,20,21,22. As a consequence of extensive exposure to tick-borne infections15,16,17, patients may develop a weakened immune system22,23, and present evidence of opportunistic infections such as Chlamydia spp.24,25,26,27, Coxsackievirus28, Cytomegalovirus29, Epstein-Barr virus27,29, Human parvovirus B1924, and Mycoplasma spp.30,31. In addition to tick-borne co-infections and non-tick-borne opportunistic infections, pleomorphic Borrelia persistent forms may induce distinct immune responses in patients by having different antigenic properties compared to typical spirochetes32,33,34,35. Nonetheless, current LD diagnostic tools do not include Borrelia persistent forms, tick-borne co-infections, and non-tick-borne opportunistic infections.
The two-tier guidelines36,37,38 for diagnosing LD by the Centers for Disease Control and Prevention (CDC) have been challenged due to the omission of co-infections and non-tick-borne opportunistic infections crucial for comprehensive diagnosis and treatment39,40. Emerging diagnostic solutions have demonstrated the usefulness of multiplex assays to test for LD and tick-borne co-infections41,42. However, these new technologies do not address seroprevalence of non-tick-borne opportunistic infections in patients suffering from TBD and they are limited to certain co-infections41,42. Non-tick-borne opportunistic microbes can manifest an array of symptoms24,29 concerning the heart, kidney, musculoskeletal, and the central nervous system as seen in patients with Lyme related carditis43, nephritis44, arthritis45, and neuropathy46, respectively. Therefore, Chlamydia spp., Coxsackievirus, Cytomegalovirus, Epstein-Barr virus, Human parvovirus B19, Mycoplasma spp., and other non-tick-borne opportunistic microbes play an important role in the differential diagnosis of LD24,29. As the current knowledge regarding non-tick-borne opportunistic microbes is limited to their use in differential diagnosis of LD, it is unclear if LD patients can present both tick-borne co-infections and non-tick-borne opportunistic infections simultaneously.
For the first time, we evaluate the involvement of Borrelia spirochetes, Borrelia persistent forms, tick-borne co-infections, and non-tick-borne opportunistic microbes together in patients suffering from different stages of TBD. To highlight the need for multiplex TBD assays in clinical laboratories, we utilized the Bradford Hill’s causal inference criteria47 to elucidate the likelihood and plausibility of TBD patients responding to multiple microbes rather than one microbe. The goal of this study is to advocate screening for various TBD microbes including non-tick-borne opportunistic microbes to decrease the rate of misdiagnosed or undiagnosed48 cases thereby increasing the health-related quality of life for the patients39, and ultimately influencing new treatment protocol for TBDs.
Results
Positive IgM and IgG responses by CDC defined acute, CDC late, CDC negative, PTLDS immunocompromised, and unspecific patients to 20 microbes associated with TBD (Fig. 1) were utilized to evaluate polymicrobial infections (Figs 2–4). Patient categories included CDC acute (n = 43), CDC late (n = 43), CDC negative (n = 46), PTLDS (n = 31), immunocompromised (n = 61), unspecific (n = 31), and healthy (n = 177).
Polymicrobial infections are present at all stages of tick-borne diseases.
Microbes include Borrelia burgdorferi sensu stricto, Borrelia afzelii, Borrelia garinii, Borrelia burgdorferi sensu stricto persistent form, Borrelia afzelii persistent form, Borrelia garinii persistent form, Babesia microti, Bartonella henselae, Brucella abortus, Ehrlichia chaffeensis, Rickettsia akari, Tick-borne encephalitis virus (TBEV), Chlamydia pneumoniae, Chlamydia trachomatis, Coxsackievirus A16 (CVA16), Cytomegalovirus (CMV), Epstein-Barr virus (EBV), Mycoplasma pneumoniae, Mycoplasma fermentans, and Human parvovirus B19 (HB19V).
In Fig. 2A, 51% and 65% of patients had IgM and IgG responses to more than one microbe, whereas 9% and 16% of patients had IgM and IgG responses to only one microbe, respectively. Immune responses to Borrelia persistent forms (all three species) for IgM and IgG were 5–10% higher compared to Borrelia spirochetes in all three species (Fig. 2B). Interestingly, the probability that a randomly selected patient will respond to Borrelia persistent forms rather than the Borrelia spirochetes (Fig. S2) is 80% (d = 1.2) for IgM and 68% for IgG (d = 0.7). Figure 2A and B indicated that IgM and IgG responses by patients from different stages of TBDs are not limited to only Borrelia spirochetes.
In Fig. 3 sub-inlets, more than 50% of the patients reacted to only the individual Borrelia strains suggesting that Borrelia antigens are not cross-reactive. If patients were cross-reacting among antigens, a larger percentage of the patients would be seen with the combination of all three species (Fig. S2). These results provide evidence to suggest that the inclusion of different Borrelia species and their morphologies in current LD diagnostic tools will improve its efficiency.
Discussions
The study outcome indicated that polymicrobial infections existed at all stages of TBD with IgM and IgG responses to several microbes (Fig. 2). Results presented in this study propose that infections in patients suffering from TBDs do not obey the one microbe one disease Germ Theory. Based on these results and substantial literature11,15,16,17,27,49,50,51 on polymicrobial infections in TBD patients, we examined the probability of a causal relationship between TBD patients and polymicrobial infections following Hill’s nine criteria47.
An average effect size of d = 1.5 for IgM and IgG (Fig. 4A) responses is considered very large52. According to common language effect size statistics53, d = 1.5 indicates 85% probability that a randomly selected patient will respond to Borrelia and other TBD microbes rather than to only Borrelia. Reports from countries such as Australia27, Germany49, Netherlands11, Sweden50, the United Kingdom51, the USA15,16, and others indicate that 4% to 60% of patients suffer from LD and other microbes such as Babesia microti and human granulocytic anaplasmosis (HGA). However, previous findings11,15,16,27,49,50,51 are limited to co-infections (i.e., Babesia, Bartonella, Ehrlichia, or Rickettsia species) in patients experiencing a particular stage of LD (such as Erythema migrans). In contrast, a broader spectrum of persistent, co-infections, and opportunistic infections associated with diverse stages of TBD patients have been demonstrated in this study (Fig. 2). From a clinical standpoint, the likelihood for IgM and IgG immune responses by TBD patients to the Borrelia spirochetes versus the Borrelia persistent forms, and responses to just Borrelia versus Borrelia with many other TBD microbes has been quantified for the first time (Fig. S2).
Borrelia pathogenesis could predispose individuals to polymicrobial infections because it can suppress, subvert, or modulate the host’s immune system18,19,20,21,22 to create a niche for colonization by other microbes54. Evidence in animals55 and humans11,15,16,27,49,50,51 frequently indicate co-existence of Borrelia with other TBD associated infections. Interestingly, IgM and IgG immune levels by patients to multiple forms of Borrelia resulted in immune responses to 14 other TBD microbes (Fig. 4B). In contrast, patient responses to either form of Borrelia (spirochetes or persistent forms) resulted in reactions to an average of 8 other TBD microbes (Fig. 4B). Reaction to two forms of Borrelia reflected an increase in disease severity indicating biological gradient for causation as required by Hill’s criteria47.
Multiple microbial infections in TBD patients seem plausible because ticks can carry more than eight different microbes depending on tick species and geography56,57. Moreover, Qiu and colleagues reported the presence of at least 18 bacterial genera shared among three different tick species and up to 127 bacterial genera in Ixodes persulcatus58. Interestingly, research indicates Chlamydia-like organism in Ixodes ricinus ticks and human skin59 that may explain immune responses to Chlamydia spp., seen in this study (Fig. 2). Additionally, prevalence of TBD associated co-infections such as B. abortus, E. chaffeensis, and opportunistic microbes such as C. pneumoniae, C. trachomatis, Cytomegalovirus, Epstein-Barr virus, and M. pneumoniae have been recorded in the general population of Europe and the USA (Table S2). However, true incidence of these microbes is likely to be higher considering underreporting due to asymptomatic infections and differences in diagnostic practices and surveillance systems across Europe and in the USA. More importantly, clinical evidence for multiple microbes has been reported in humans11,15,16,27,49,50,51, and livestock55 to mention the least. Our findings regarding the presence of polymicrobial infections at all stages of TBD further supports the causal relationship between TBD patients and polymicrobial infections (Fig. 2). Various microbial infections in TBD patients have been linked to the reduced health-related quality of life (HRQoL) and increased disease severity39.
An association between multiple infections and TBD patients relates well to other diseases such as periodontal, and respiratory tract diseases. Oral cavities may contain viruses and 500 different bacterial species60. Our findings demonstrate that TBD patients may suffer from multiple bacterial and viral infections (Fig. 4). In respiratory tract diseases, influenza virus can stimulate immunosuppression and predispose patients to bacterial infections causing an increase in disease severity61. Likewise, Borrelia can induce immunosuppression that may predispose patients to other microbial infections causing an increase in disease severity.
Traditionally, positive IgM immune reaction implies an acute infection, and IgG response portrays a dissemination, persistent or memory immunity due to past infections. Depending on when TBD patients seek medical advice, the level of anti-Borrelia antibodies can greatly vary as an Erythema migrans (EM) develops and may present with IgM, IgG, collective IgM/IgG, or IgA62. This study recommends both IgM and IgG in diagnosing TBD (Figs 5 and S4–S6) as unconventional antibody profiles have been portrayed in TBD patients. Presence of long-term IgM and IgG antibodies have been reported in LD patients that were tested by the CDC two-tier system. In 2001, Kalish and colleagues reported anti-Borrelia IgM or IgG persistence in patients that suffered from LD 10–20 years ago63. Similarly, Hilton and co-workers recorded persistent anti-Borrelia IgM response in 97% of late LD patients that were considered cured following an antibiotic treatment64.
Similar events of persistent IgM and IgG antibody reactions were demonstrated in patients treated for Borrelia arthritis and acrodermatitis chronica atrophicans65, chronic cutaneous borreliosis66, and Lyme neuroborreliosis67. A clear phenomenon of immune dysfunction is occurring, which might account for the disparities in LD patient’s antibody profiles and persistence. Borrelia suppresses the immune system by inhibition of antigen-induced lymphocyte proliferation18, reducing Langerhans cells by downregulation of major histocompatibility complex class II molecules on these cells19, stimulating the production of interleukin-10 and anti-inflammatory immunosuppressive cytokine20, and causing disparity in regulation and secretion of cytokines21. Other studies have demonstrated low production or subversion of specific anti-Borrelia antibodies in patients with immune deficiency status22.
In the USA alone, the economic healthcare burden for patients suffering from LD and ongoing symptoms is estimated to be $1.3 billion per year69. Additionally, 83% of all TBD diagnostic tests performed by the commercial laboratories in the USA accounted for only LD70. Globally, the commercial laboratories’ ability to diagnose LD has increased by merely 4% (weighted mean for ELISA sensitivity 62.3%) in the last 20 years71. This study provides evidence regarding polymicrobial infections in patients suffering from different stages of TBDs. Literature analyses and results from this study followed Hill’s criteria indicating a causal association between TBD patients and polymicrobial infections. Also, the study outcomes indicate that patients may not adhere to traditional IgM and IgG responses.
__________________
**Comment**
For the first time, Garg et al. show a 85% probability for multiple infections including not only tick-borne pathogens but also opportunistic microbes such as EBV and other viruses.
I’m thankful they included Bartonella as that one is often omitted but definitely a player. I’m also thankful for the mention of viruses as they too are in the mix. The mention of the persister form must be recognized as well as many out there deny its existence.
Key Quote: “Our findings recognize that microbial infections in patients suffering from TBDs do not follow the one microbe, one disease Germ Theory as 65% of the TBD patients produce immune responses to various microbes.”
But there is another important point.
According to this review, 83% of all commercial tests focus only on Lyme (borrelia), despite the fact we are infected with more than one microbe. The review also states it takes 11 different visits to 11 different doctors, utilizing 11 different tests to be properly diagnosed. https://www.news-medical.net/news/20181101/Tick-borne-disease-is-multiple-microbial-in-nature.aspx?