https://www.thefocalpoints.com/p/breaking-american-academy-of-pediatrics?
BREAKING: American Academy of Pediatrics Hit With Federal RICO Lawsuit for Vaccine Safety Fraud
AAP accused of operating a decades-long racketeering scheme that deceived America about vaccine safety for maximum profit.
For decades, the American Academy of Pediatrics (AAP) has been treated like an untouchable authority on child health — the gold standard that parents, doctors, schools, and lawmakers were told to trust without question. But today, that image collapses. Children’s Health Defense (CHD) and multiple plaintiffs just filed a federal lawsuit alleging the AAP spent decades running a racketeering operation that sold parents false safety assurances about the childhood vaccine schedule.
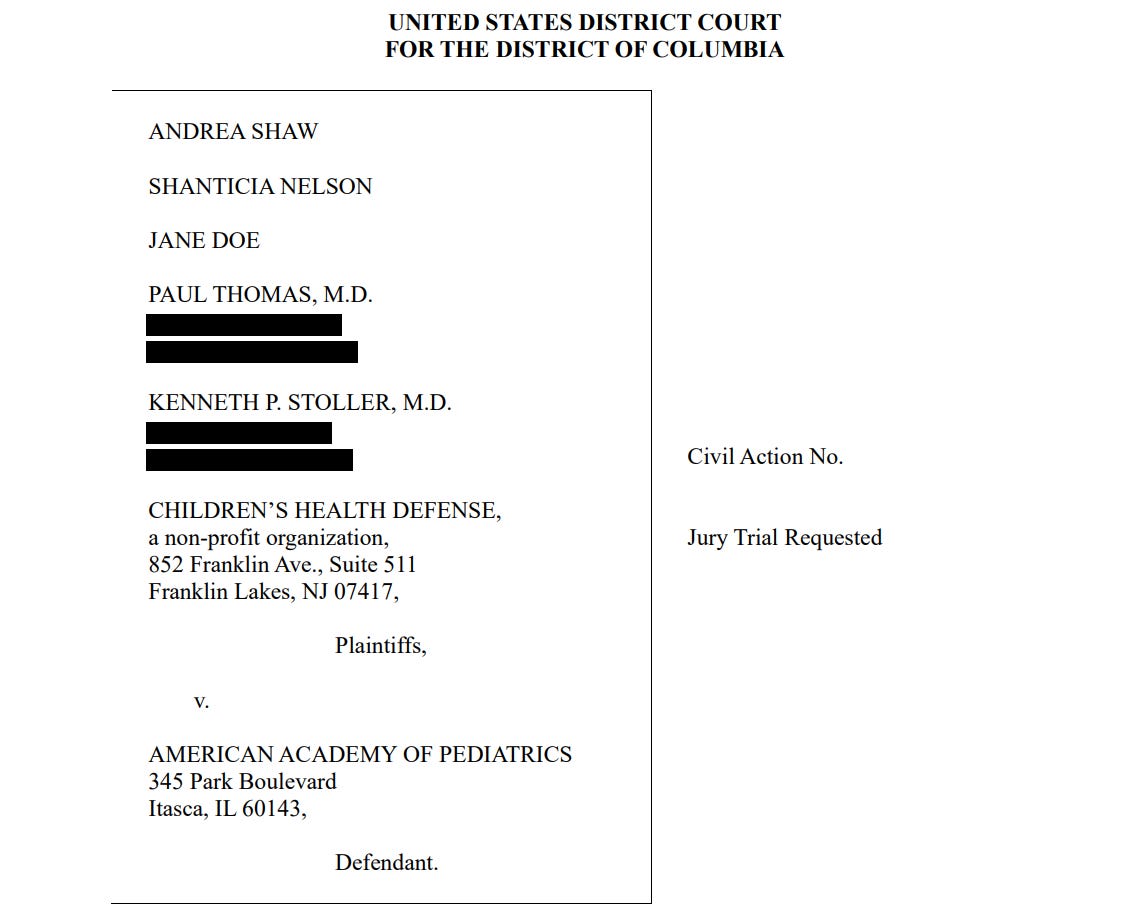
This isn’t another “vaccine debate” lawsuit. It’s a RICO fraud case—the same legal weapon used against organized crime and the tobacco industry. The allegation is blunt and devastating: the AAP allegedly manufactured false certainty around vaccine schedule safety, shut down legitimate scientific scrutiny, and promoted sweeping assurances that were never validated through rigorous real-world safety testing—while operating within a system shaped by vaccine-manufacturer funding and financial incentives tied to high pediatric vaccination rates.
One of the most explosive points in the complaint is what it forces into the open. The cumulative childhood schedule has never been safety-tested the way any reasonable parent would assume it has. The lawsuit points to Institute of Medicine findings from 2002 and 2013 calling for more research and acknowledging the lack of proper vaccinated vs. unvaccinated comparisons. Yet the AAP continued portraying the schedule as thoroughly tested and unquestionably safe, shaping pediatric care nationwide through repetition, authority, and pressure—not proof.
The complaint also describes what parents have learned the hard way. This system doesn’t merely recommend vaccines. It demands compliance. Physicians who questioned the schedule or deviated from AAP protocols were professionally targeted, disciplined, and financially crushed. The message was clear: follow the script, or lose your career.
The lawsuit further argues that the AAP’s public reassurances were built on “theoretical” talking points that became institutional doctrine, including the infamous claim that infants could tolerate an extreme number of vaccines at once. According to the plaintiffs, this wasn’t evidence—it was marketing disguised as medical authority, repeated in clinics to silence questions and keep the assembly line moving.
Then there’s the part that makes it all make sense: money. The complaint highlights conflicts of interest and financial entanglements with vaccine manufacturers and aligned institutions. The AAP presents itself as independent and science-first, while operating in a world of corporate sponsorships, incentives, and industry relationships that would be unacceptable in any genuinely transparent public health organization.
This is why the lawsuit matters. It’s not about a single product. It challenges the entire protection racket that has propped up the pediatric vaccine industry for decades. AAP’s model has relied on one rule: the schedule is safe because we say it’s safe—and anyone who demands real proof gets smeared, censored, or destroyed.
The lawsuit seeks financial damages for the families and physicians harmed, demands disclosure of the lack of comprehensive safety testing behind the cumulative schedule, and aims to stop the AAP from making blanket, unqualified claims that the schedule is “safe and effective” as if that question has already been settled.
If this case advances, discovery alone could expose what the public has been denied for decades—and that would be a historic victory for medical transparency, informed consent, and accountability in pediatrics. For years, parents were told to “trust the experts,” while legitimate safety questions were mocked, censored, or punished. Now those questions are headed to the one place the system can’t silence them with talking points: federal court. (See link for article)
____________
- The AAP is completely and utterly corrupt: https://madisonarealymesupportgroup.com/2026/01/15/the-war-over-your-medical-rights-aap-sues-rfk-while-ima-seeks-to-end-medical-mandates/
- https://madisonarealymesupportgroup.com/2022/12/09/the-real-agenda-behind-the-american-academy-of-pediatrics-weaponizing-childrens-mental-health-and-vaccines-for-profit/
For more:
- https://madisonarealymesupportgroup.com/2018/03/17/kids-dying-after-vaccinations/ A Century of Evidence Vaccines Cause SIDS
- https://madisonarealymesupportgroup.com/2019/01/07/the-vaccine-debate-top-government-expert-states-vaccines-can-cause-autism-in-some-children/
- https://madisonarealymesupportgroup.com/2026/01/05/cdc-shrinks-childhood-vaccine-schedule-by-55-doses/
- https://madisonarealymesupportgroup.com/2020/12/31/vaccinated-vs-unvaccinated-the-study-the-cdc-refused-to-do/
- https://madisonarealymesupportgroup.com/2023/10/10/vaccinated-vs-unvaccinated-kids-the-data-how-many-vaccine-coincidences-will-it-take-until-the-truth-is-accepted/
- https://madisonarealymesupportgroup.com/2018/09/08/acip-vote-yes-for-new-vaccine-despite-no-safety-studies-on-cumulative-effect-with-other-vaccines/
- https://madisonarealymesupportgroup.com/2025/12/17/peer-reviewed-reanalysis-of-henry-ford-birth-cohort-study-finds-vaccinated-children-sicker-across-all-22-chronic-disease-categories/
- https://madisonarealymesupportgroup.com/2019/08/05/fully-vaccinated-vs-unvaccinated-a-summary-of-the-research/
- https://madisonarealymesupportgroup.com/2020/06/03/new-research-study-clarifies-health-outcomes-in-vaccinated-versus-unvaccinated-children/
- https://madisonarealymesupportgroup.com/2025/12/11/fda-investigating-deaths-potentially-linked-to-covid-19-vaccines/
- https://madisonarealymesupportgroup.com/2023/10/25/yes-insurance-companies-pay-doctors-to-vaccinate-kids-now-they-are-using-virtual-reality-to-get-the-job-done/
- https://madisonarealymesupportgroup.com/2025/12/17/more-toddlers-dead-after-vaccinations-mom-warns-others-dont-blindly-follow-cdc-schedule/
- https://madisonarealymesupportgroup.com/2026/01/12/welcome-to-clown-world-bayer-sues-pfizer-moderna-for-using-monsantos-patented-gmo-technology-to-build-covid-vaccines-which-are-indistinguishable-from-bio-chemical-weapons/


