Aluminum in the Brain in Multiple Sclerosis: Regulatory and Funding Agencies Silent, Complicit
By James Lyons Weiler in Cures August 18, 2018
MEDICAL SCIENCE proceeds along a hierarchy of evidence; often, patients are studied individually (case studies), or a small collection of patients are examined and characterized together (case series studies). Case series studies typically have smallish sample sizes and it is generally understood that larger studies will be necessary to determine more accurately the characteristics being studied.
In a new case series study, brain tissue from 14 donors with a diagnosis of MS was studied in a case series by Mold et al (2018) using transversely heated graphite furnace atomic absorption spectrometry. The study found high aluminum content (>10 ug/g dry weight) in all areas of the brain studied, with some areas exceeding 50 ug/g. They found aluminum both with cells and in the interstitium between cells. They found aluminum co-localised with structures known to be present in Secondary Progressive Multiple Sclerosis (SPMS) in the frontal cortex of one donor with SPMS.
There are a number of critical lines of evidence that make this fundamental finding critically important. Patients with MS have lower amounts of aluminum in their hair, suggesting depressed detoxification, and higher amounts are found in urine on chelation challenge testing (Fulgenzi et al., 2014). Chelation with EDTA is known to significantly reduce aluminum intoxication (Fulgenzi et al. 2014), and consumption of silica-rich mineral waters also increase urinary excretion of aluminum from patients with SPMS (Jones et al., 2017).
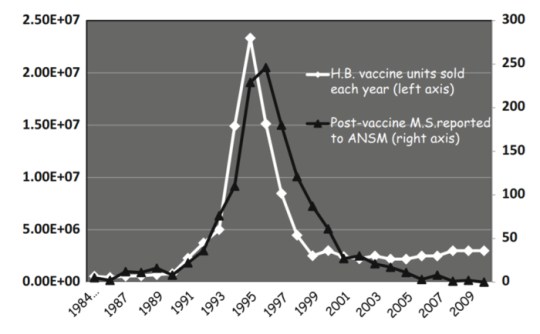
Extremely plausible direct mechanisms of the cause of MS from aluminum are known and animal studies routinely induced MS using aluminum hydroxide injections. So much evidence exists that points to aluminum as a source of strange new conditions of unknown causes, such as MMF and Gulf War Syndrome, one would think that calls to reconsider the use of aluminum in vaccines would be answered. The same team had previously found high amounts of aluminum in the brains of people with autism, and and in patients with Alzheimer’s disease. The latter result, while also important, is not surprising, as it has long been known that amyloid is part protein and part aluminum. Finally, when France brought on HepB vaccination, cases of MS following vaccination increased; when they stopped recommending the HepB vaccine, which contains aluminum hydroxide, the rate of HepB vaccine-associated MS cases dropped to near zero.
Complicity
What is surprising is the lack of action on the part of the US FDA to put an end to the use of this dangerous metal in vaccines, and that the NIH is not funding more studies like this. NIH should fund studies to determine how to most safely remove aluminum from anyone exposed via vaccines; brain stem amyloidosis is a non-trivial concern. Approaches like ketogenic diet, silica-rich mineral waters, hyperbaric oxygen, EDTA, intranasal insulin and intranasal deferoxamine (to prevent brain stem amyloidosis) should all be tested in randomized clinical trails in clinical populations known to be afflicted with aluminum intoxication (autism, Alzheimer’s, MS).
What is also surprising is that the CDC and ACIP remain blithe to the morbidity and mortality their continued approval of vaccines that contain metals like aluminum and mercury. They make decisions on behalf of us all, and yet every member of ACIP with the exception of one military member has conflicts of interest with vaccine manufacturers. ACIP should review all of the literature on aluminum and make recommendations on how to phase it, and thimerosal, out of vaccines completely.
Further inaction on the part of these regulatory and funding agencies, and active denialism at this point will surely be seen by future generations as both callous disregard, and where conflicts of interest reside, complicity.
The study, conducted at the Keele University, was funded in part by the Children’s Medical Safety Research Institute.
References
Jones K et al. EBioMedicine. 2017 Urinary Excretion of Aluminium and Silicon in Secondary Progressive Multiple Sclerosis. 26:60-67. doi: 10.1016/j.ebiom.2017.10.028.
Fulgenzi A, Vietti D1, Ferrero ME. Aluminium involvement in neurotoxicity. Biomed Res Int. 2014;2014:758323. doi: 10.1155/2014/758323.
_______________
**Comment**
https://www.nationalmssociety.org/Symptoms-Diagnosis/Other-Conditions-to-Rule-Out/Lyme-Disease
Lyme disease can cause delayed neurologic symptoms similar to those seen in multiple sclerosis (MS) such as weakness, blurred vision caused by optic neuritis, dysesthesias (sensations of itching, burning, stabbing pain, or “pins and needles”), confusion and cognitive dysfunction, and fatigue. Lyme disease symptoms may also have a relapsing-remitting course. In addition, Lyme disease occasionally produces other abnormalities that are similar to those seen in MS, including positive findings on magnetic resonance imaging (MRI) scans of the brain and analysis of cerebrospinal fluid (CSF).
These similarities in symptoms and test results have led some people with MS to seek testing for the presence of antibodies to Borrelia, to determine if their neurologic symptoms are the result of Lyme disease or truly MS. The distinction is important because Lyme disease, especially when treated early, often responds to antibiotic therapy, whereas MS does not.
Studies examining Lyme disease & MS
Two studies have examined the overlap in diagnosis of MS and Lyme disease. The studies were conducted in parts of Long Island, New York, an area where Lyme disease is endemic, or regularly found.
In the first study, people who had Borrelia antibodies in their blood as well as a variety of neurologic symptoms considered to be “MS-like,” were evaluated with MRI, evoked potentials (EP) and CSF analysis, including a test for the presence of Borrelia antibodies in the spinal fluid.
While those with the MS-like illness had the highest incidence of abnormal MRIs and were the only ones among those studied to have abnormal EP and oligoclonal bands in their spinal fluid (indicating an abnormal immune response), they did not prove to have any Borrelia antibody in their spinal fluid.
The researchers concluded that the few patients with the MS-like symptoms probably had these symptoms due to MS and had also been exposed to the Borrelia bacterium.
A companion study looked for the presence of Borrelia antibodies in the blood of 100 people with the diagnosis of possible MS. Of 89 people who in fact turned out to have definite MS, only one had Borrelia antibodies. The researcher concluded that “…infection with Borrelia is infrequent in MS patients who live in an endemic area. Lyme disease is unlikely to be a significant factor in the differential diagnosis of MS.” Furthermore, the presence or antibodies to Borrelia does not prove that Borrelia is causing the neurological symptoms, only that there has been previous infection with the organism.
Just remember, “rare” is only “rare” if it isn’t you.