Chronic inflammation removes motivation by reducing dopamine in the brain
June 5, 2109
Written by Dr. Liji Thomas
Why do we feel listless when we are recovering from an illness? The answer is, apparently, that low-grade chronic inflammation interferes with the dopaminergic signaling system in the brain that motivates us to do things.
This was reported in a new paper published in the journal Trends in Cognitive Sciences.
The research carried out at Emory University explains the links between the reduced release of dopamine in the brain, the motivation to do things, and the presence of an inflammatory reaction in the body. It also presents the possibility that this is part of the body’s effort to optimize its energy expenditure during such inflammatory episodes, citing evidence gathered during their study.
The authors also published an experimental framework based on computational tools, devised to test the theory.
The underlying hypothesis is that the body needs more energy to heal a wound or overcome an infection, for instance, both of which are associated with low-grade inflammation. To ensure that energy is available, the brain uses an adaptive technique to reduce the natural drive to perform other tasks which could potentially drain away the energy needed for healing. This is essentially a recalibration of the specialized reward neurons in the motivation center of the brain, so that ordinary tasks no longer feel like they’re worth doing.
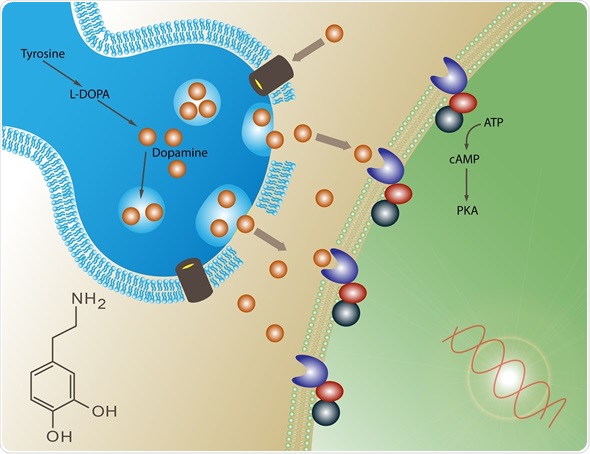
According to the new study, the mechanism of this recalibration is immune-mediated disruption of the dopamine pathway, reducing dopamine release.
The computational technique published by the scientists is designed to allow experimental measurements of the extent to which low-grade inflammation affects the amount of energy available, and the decision to do something based on the effort needed. This could allow us to better understand why and how chronic inflammatory states cause a lack of motivation in other disease conditions as well, including schizophrenia and depression.
Andrew Miller, co-author of the study, says,
“If our theory is correct, then it could have a tremendous impact on treating cases of depression and other behavioral disorders that may be driven by inflammation. It would open up opportunities for the development of therapies that target energy utilization by immune cells, which would be something completely new in our field.”
It is already known that immune cells release cellular signaling molecules called cytokines, which affect the functioning of the dopamine-releasing neurons in the area of the brain called the mesolimbic system. This area enhances our willingness to work hard for the sake of a reward.
Source: Treadway M. T. et al., (2019). Can’t or Won’t? Immunometabolic Constraints on Dopaminergic Drive. Trends in Cognitive Sciences. https://doi.org/10.1016/j.tics.2019.03.003
________________
Lyme and Dopaminergic Function: Hypothesizing Reduced Reward Deficiency Symptomatology by Regulating Dopamine Transmission.
Abstract
The principal vector of Lyme disease in the United States is Ixodes scapularis: black legged or deer ticks. There is increased evidence that those infected may be plagued by anxiety or depression as well. Researchers have identified transcripts coding for two putative cytosolic sulfotransferases in these ticks, which recognized phenolic monoamines as their substrates. It is hypothesized that protracted Lyme disease sequelae may be due to impairment of dopaminergic function of the brain reward circuitry. The subsequent recombinant proteins exhibited sulfotransferase function against two neurotransmitters: dopamine and octopamine. This, in itself, can reduce dopamine function leading to many Reward Deficiency Syndrome behaviors, including depression and possibly, anxiety. In fact, it was shown that activity of Ixosc Sult 1 and Sult 2 in the Ixodid tick salivary glands might contain inactivation of the salivation signal through sulfonation of either dopamine or octopamine. This infraction results in a number of clinically observed mood changes, such as anxiety and depression. In fact, there are common symptoms observed for both Parkinson and Lyme diseases. The importance of understanding the mechanistic and neurobiological effects of Lyme on the central nervous system (CNS) provides the basis for pro-dopamine regulation as a treatment. WC 195.
Great article on dopamine: https://suzycohen.com/articles/depression_low_dopamine/ Excerpt:
Dopamine deficiency will cause you to wake up sluggish in the morning, usually with brain fog, but you might feel happier and suddenly more enthusiastic with a “hit” of some sort, perhaps a cup of coffee. Low dopamine (as opposed to low serotonin) causes a different kind of depression, one that is hallmarked by a lack of pleasure.
